The Origins of AIDS (18 page)
Read The Origins of AIDS Online
Authors: Pepin

Such once-a-week regimens were quite manageable as nurses left behind by the mobile teams could rotate between villages, treating all cases in a given village on Mondays, all cases in a second village on Tuesdays and so on, repeating this circuit twelve times. This mobility of
practical nurses implied that the procedures for sterilising syringes and needles were minimal. However, they became extremely skilled at giving IV injections, as is evident in a movie about Jamot made in
1932, which can be downloaded from
www.creuse-jamot.org/html/1931-1935.html
. This film provides an extraordinary illustration of the scope of the sleeping sickness problem in Cameroun and of the methods used for its control.
practical nurses implied that the procedures for sterilising syringes and needles were minimal. However, they became extremely skilled at giving IV injections, as is evident in a movie about Jamot made in
1932, which can be downloaded from
www.creuse-jamot.org/html/1931-1935.html
. This film provides an extraordinary illustration of the scope of the sleeping sickness problem in Cameroun and of the methods used for its control.
Some trypanosomiasis patients who relapsed after standard therapy also received
hétérohémothérapie
: the repeated IM administration of 10–20 cc of whole blood from convalescent patients. The idea was that this blood contained high levels of antibodies against trypanosomes, which would be useful to patients who had difficulty getting rid of the parasite. Although this was certainly a good method for transmitting viral infectious agents (because the quantity of blood deliberately administered was much larger than whatever was inadvertently left in a syringe after it was flushed), it was probably not used on more than 1,000 patients.
13
,
28
hétérohémothérapie
: the repeated IM administration of 10–20 cc of whole blood from convalescent patients. The idea was that this blood contained high levels of antibodies against trypanosomes, which would be useful to patients who had difficulty getting rid of the parasite. Although this was certainly a good method for transmitting viral infectious agents (because the quantity of blood deliberately administered was much larger than whatever was inadvertently left in a syringe after it was flushed), it was probably not used on more than 1,000 patients.
13
,
28
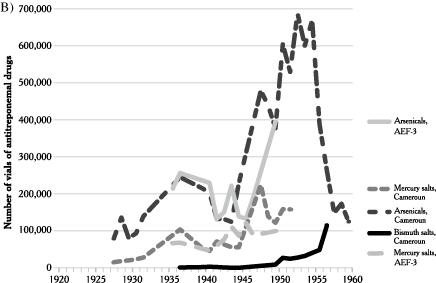
Data on the incidence of various diseases must be viewed with caution from a purely epidemiological perspective because year-to-year variations may reflect the more or less intense efforts made to find cases rather than true changes. For instance, the rising incidence of sleeping sickness in Cameroun around 1928 reflected the increasing resources devoted to its control: mobile teams explored areas where hitherto most cases had remained undiagnosed, unreported and untreated. However, even if imperfect for reconstructing disease dynamics, these data reflect accurately the numbers of patients treated with injectable drugs given for specific diseases.
In Cameroun, the incidence of sleeping sickness peaked at 54,712 new cases in 1928 (
Figure 10
). The disease was concentrated in a triangle east of Yaoundé (Akonolinga,
Abomg-Mbang and Doumé) where in some communities almost everyone had to be treated. The incidence then decreased and stabilised at around 3,000 cases per year until 1952. The decline during WWII reflected reduced human and material resources for case-finding, as several of the medical officers were mobilised into general Leclerc’s Free French Forces.
24
,
25
,
29
,
30
Figure 10
). The disease was concentrated in a triangle east of Yaoundé (Akonolinga,
Abomg-Mbang and Doumé) where in some communities almost everyone had to be treated. The incidence then decreased and stabilised at around 3,000 cases per year until 1952. The decline during WWII reflected reduced human and material resources for case-finding, as several of the medical officers were mobilised into general Leclerc’s Free French Forces.
24
,
25
,
29
,
30
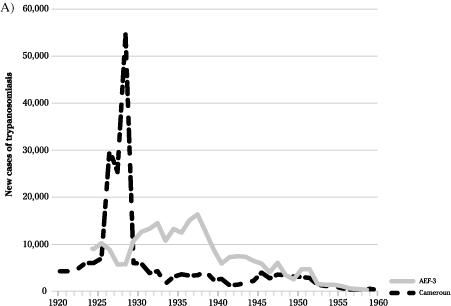
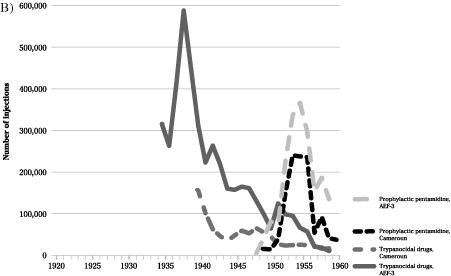
Figure 10
Incidence of African trypanosomiasis (sleeping sickness) in Cameroun Français and AEF-3, and use of trypanocidal drugs.
Incidence of African trypanosomiasis (sleeping sickness) in Cameroun Français and AEF-3, and use of trypanocidal drugs.
Adapted from Pepin.
10
10
In AEF-3, incidence of trypanosomiasis peaked in 1937 and the number of injections of trypanocidal drugs followed the same course, peaking at a staggering 588,086 injections. During the years for which detailed information is available, 74% of the 3.9 million injections used
in the treatment of sleeping sickness were given IV (
tartar emetic,
suramin,
tryparsamide,
melarsoprol), 3% IM (
pentamidine), 13% SC (
atoxyl,
trypoxyl) and for 10% the route is uncertain (
orsanine). As discussed in the
previous chapter
, the IV injections provided the best opportunities for the transmission of blood-borne viruses.
10
in the treatment of sleeping sickness were given IV (
tartar emetic,
suramin,
tryparsamide,
melarsoprol), 3% IM (
pentamidine), 13% SC (
atoxyl,
trypoxyl) and for 10% the route is uncertain (
orsanine). As discussed in the
previous chapter
, the IV injections provided the best opportunities for the transmission of blood-borne viruses.
10
Apart from the short epidemic period in Cameroun, the annual incidence rates of trypanosomiasis were lower than 10 per 1,000 inhabitants (
Figure 11
). Thus the number of individuals who could have been iatrogenically infected with blood-borne viruses during trypanosomiasis treatment in colonial Cameroun was substantial (about 222,000), but not high enough by itself to result in the extremely high prevalence of hepatitis
C (more than 40%) described much later throughout southern Cameroon, which must have resulted from a combination of interventions rather than from a single one
.
Figure 11
). Thus the number of individuals who could have been iatrogenically infected with blood-borne viruses during trypanosomiasis treatment in colonial Cameroun was substantial (about 222,000), but not high enough by itself to result in the extremely high prevalence of hepatitis
C (more than 40%) described much later throughout southern Cameroon, which must have resulted from a combination of interventions rather than from a single one
.
However, we need just one of the trypanosomiasis patients to have been infected with SIV
cpz
, acquired while manipulating chimpanzee carcasses, to initiate a chain of transmission that could have exponentially amplified the number of infected individuals. And the peak period for trypanosomiasis incidence and its injectable treatments, the late 1920s, corresponded closely, give or take a few years, to the dating of the most recent common ancestors of HIV-1 group M.
cpz
, acquired while manipulating chimpanzee carcasses, to initiate a chain of transmission that could have exponentially amplified the number of infected individuals. And the peak period for trypanosomiasis incidence and its injectable treatments, the late 1920s, corresponded closely, give or take a few years, to the dating of the most recent common ancestors of HIV-1 group M.
A new intervention,
pentamidinisation
, was launched in 1948. IM pentamidine, then a novel drug, was administered to the whole population of endemic areas as a preventive measure. Pentamidine was later used in the treatment of
Pneumocystis
pneumonia and, as seen in the introduction, an abnormal blip in its use played a role in the recognition of AIDS as a new disease in the US in 1981. Scientists of the colonial era mistakenly thought that pentamidine persisted long enough in the blood for a single injection to provide levels sufficient to abort infections with trypanosomes that might ensue over the following semester. In reality, there was little pentamidine remaining in the body two weeks later. In the early 1950s, more than half a million injections of pentamidine were given annually in French territories of central Africa (
Figure 10
).
Pentamidinisation
contributed to a further reduction in the incidence of sleeping sickness, not because it was truly preventive, but because single-dose pentamidine was curative for patients with recently acquired, often asymptomatic, trypanosomiasis.
31
pentamidinisation
, was launched in 1948. IM pentamidine, then a novel drug, was administered to the whole population of endemic areas as a preventive measure. Pentamidine was later used in the treatment of
Pneumocystis
pneumonia and, as seen in the introduction, an abnormal blip in its use played a role in the recognition of AIDS as a new disease in the US in 1981. Scientists of the colonial era mistakenly thought that pentamidine persisted long enough in the blood for a single injection to provide levels sufficient to abort infections with trypanosomes that might ensue over the following semester. In reality, there was little pentamidine remaining in the body two weeks later. In the early 1950s, more than half a million injections of pentamidine were given annually in French territories of central Africa (
Figure 10
).
Pentamidinisation
contributed to a further reduction in the incidence of sleeping sickness, not because it was truly preventive, but because single-dose pentamidine was curative for patients with recently acquired, often asymptomatic, trypanosomiasis.
31
A description of the
pentamidinisation
procedures gives an idea of the potential for transmission of blood-borne pathogens:
pentamidinisation
procedures gives an idea of the potential for transmission of blood-borne pathogens:
The principles of mass production and time and motion study should be applied to ensure the maximum speed and efficiency in getting through, say, 250 injections in a morning. The man actually giving the injection should merely have to turn around in order to hand over his used syringe and take a freshly charged one. As he turns back again, a freshly iodined buttock, and the appropriate dose, should present themselves before him.
32
Pentamidinisation
was discontinued as endemic countries approached their independence. The injections were extremely painful, unpopular and associated with colonial rule. And as the incidence of trypanosomiasis declined further, priority was given to more pressing health needs, such as leprosy which had hitherto been neglected. Furthermore, outbreaks of gas gangrene (an infection that causes necrosis of the muscles, with a very high mortality rate) occurred in Gabon, Cameroun and Oubangui-Chari. Pentamidine bulk powder was diluted with locally procured water, some of which had been contaminated with
Clostridium
spores, which are very hard to kill. Dozens of deaths among healthy individuals as a consequence of a preventive intervention were unacceptable to local populations.
was discontinued as endemic countries approached their independence. The injections were extremely painful, unpopular and associated with colonial rule. And as the incidence of trypanosomiasis declined further, priority was given to more pressing health needs, such as leprosy which had hitherto been neglected. Furthermore, outbreaks of gas gangrene (an infection that causes necrosis of the muscles, with a very high mortality rate) occurred in Gabon, Cameroun and Oubangui-Chari. Pentamidine bulk powder was diluted with locally procured water, some of which had been contaminated with
Clostridium
spores, which are very hard to kill. Dozens of deaths among healthy individuals as a consequence of a preventive intervention were unacceptable to local populations.
One of these
iatrogenic tragedies, in
Nkoltang, Gabon, where fourteen pentamidine recipients died of gas gangrene in 1952, provided an extraordinary example of the work of colonial spin doctors. While the inquiry revealed in confidential documents that the fault lay with the French nurse who did not properly sterilise the water that he had secured from a local source, which was itself contaminated with surface water, the official reports blamed the unfortunate recipients who were alleged to have applied some mud at the site of the injection as a pain- relieving method
. This makes us wonder whether other iatrogenic complications, for instance outbreaks of ‘inoculation hepatitis’, would have been reported
.
33
–
34
iatrogenic tragedies, in
Nkoltang, Gabon, where fourteen pentamidine recipients died of gas gangrene in 1952, provided an extraordinary example of the work of colonial spin doctors. While the inquiry revealed in confidential documents that the fault lay with the French nurse who did not properly sterilise the water that he had secured from a local source, which was itself contaminated with surface water, the official reports blamed the unfortunate recipients who were alleged to have applied some mud at the site of the injection as a pain- relieving method
. This makes us wonder whether other iatrogenic complications, for instance outbreaks of ‘inoculation hepatitis’, would have been reported
.
33
–
34
Chronologically, after trypanosomiasis, yaws and syphilis were the next diseases for the treatment of which huge numbers of injections were administered. They are caused by two subspecies of the same bacterium,
Treponema pallidum
, and are referred to as treponemal diseases, treated with antitreponemal drugs.
Yaws, caused by
Treponema pallidum pertenue
, is transmitted by non-sexual direct contacts. Its principal manifestation, skin lesions, can be spectacular, but there are few long-term complications. Its incidence was highest in children living in the forested areas of central Africa. In some populations mothers were deliberately infecting their children by inducing contacts with obvious cases so that their kids would develop immunity to yaws
.
On the other hand, sexually transmitted syphilis is caused by
Treponema pallidum pallidum
. It causes ulceration of the genitalia, after which it disseminates via the bloodstream, also causing skin lesions and later involvement of other organs including the aorta and the brain
.
Both infections were treated with
arsenic-,
bismuth- or
mercury-based compounds and, since the mid-1950s,
penicillin. Diagnoses of yaws were reasonably accurate because of the prominence of cutaneous signs. Although many diagnoses of syphilis, made without testing by nurses with only basic training, were doubtful (according to the health officials who wrote the reports), these patients were treated as if they indeed had syphilis
.
35
–
36
Treponema pallidum
, and are referred to as treponemal diseases, treated with antitreponemal drugs.
Yaws, caused by
Treponema pallidum pertenue
, is transmitted by non-sexual direct contacts. Its principal manifestation, skin lesions, can be spectacular, but there are few long-term complications. Its incidence was highest in children living in the forested areas of central Africa. In some populations mothers were deliberately infecting their children by inducing contacts with obvious cases so that their kids would develop immunity to yaws
.
On the other hand, sexually transmitted syphilis is caused by
Treponema pallidum pallidum
. It causes ulceration of the genitalia, after which it disseminates via the bloodstream, also causing skin lesions and later involvement of other organs including the aorta and the brain
.
Both infections were treated with
arsenic-,
bismuth- or
mercury-based compounds and, since the mid-1950s,
penicillin. Diagnoses of yaws were reasonably accurate because of the prominence of cutaneous signs. Although many diagnoses of syphilis, made without testing by nurses with only basic training, were doubtful (according to the health officials who wrote the reports), these patients were treated as if they indeed had syphilis
.
35
–
36
Figure 11
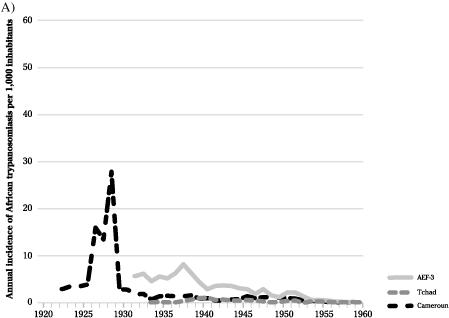
Incidence rates (per 1,000 inhabitants per year) of African trypanosomiasis, yaws and syphilis in Cameroun Français, AEF-3 and Tchad.
Adapted from Pepin.
10
10
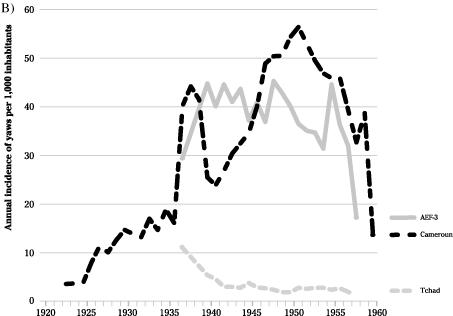
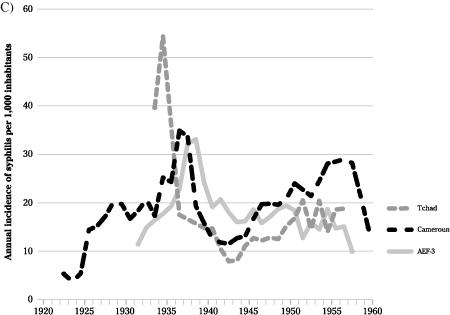
In Cameroun, the incidence of yaws increased dramatically in 1936, decreased transiently during WWII, peaked at 172,693 new cases in 1950 and slowly declined thereafter (
Figure 12
). For syphilis, a less marked biphasic pattern was seen. Throughout this period, annual
incidence rates of yaws varied between 24 and 56 per 1,000 inhabitants; incidence of syphilis was lower, between 12 and 35 per 1,000 (
Figure 11
). In AEF-3, yaws peaked at 96,898 cases in 1954, while syphilis peaked earlier. Incidence rates of yaws were much lower in
Tchad than in AEF-3 or Cameroun, while there was little geographic variation for syphilis (
Figure 11
). Incidence rates of yaws and syphilis were highest in
Gabon, where the ecological conditions facilitated the transmission of the former disease, while behaviours facilitated the latter.
Figure 12
). For syphilis, a less marked biphasic pattern was seen. Throughout this period, annual
incidence rates of yaws varied between 24 and 56 per 1,000 inhabitants; incidence of syphilis was lower, between 12 and 35 per 1,000 (
Figure 11
). In AEF-3, yaws peaked at 96,898 cases in 1954, while syphilis peaked earlier. Incidence rates of yaws were much lower in
Tchad than in AEF-3 or Cameroun, while there was little geographic variation for syphilis (
Figure 11
). Incidence rates of yaws and syphilis were highest in
Gabon, where the ecological conditions facilitated the transmission of the former disease, while behaviours facilitated the latter.
Within Cameroun, there was little regional variation in the incidence rates of syphilis, but dramatic variations in the incidence of yaws, sometimes measured at over 200 per 1,000 inhabitants per year in the southern regions (where almost the whole population would be treated, mostly with injectable drugs, over just a few years) compared to less than 1 per 1,000 in the north. Coincidentally, the regions hyperendemic for yaws corresponded to the habitat of
P.t. troglodytes
.
P.t. troglodytes
.
Several therapeutic regimens with three to fifteen injections of metallic drugs were used: (i) arsenicals: IV novarsenobenzol, IV fontarsol, IM acetylarsan, IM sulpharsenol or oral stovarsol (children only); (ii) IM bismuth salts; or (iii) IV or IM mercury salts. Combination therapies made it possible to shorten the duration of treatment. Overall, patients received fewer injections than planned as some did not return when their skin lesions improved (in contrast with trypanosomiasis for which patients felt the need to receive all intended injections to improve their chances of survival).
37
–
40
37
–
40
Data on consumption of antitreponemal drugs were more exhaustive for Cameroun, where the use of parenteral arsenicals increased dramatically, up to 688,750 vials in 1952 (
Figure 12
), in parallel with a rising incidence and better funding after the war. Overall, 51% of parenteral arsenicals used against yaws were administered IV. For bismuth salts,
Figure 12
shows the numbers of vials. However, most of the bismuth came as bulk powder, which was then diluted locally with water. For 1952–4, it can be calculated that some 500,000 additional injections of bismuth were made each year. In AEF-3, use of parenteral arsenicals doubled to 394,189 vials in 1949; there is little information about bismuth
. Mercury salts, cheaper but much more toxic, were abandoned in 1951
.
Figure 12
), in parallel with a rising incidence and better funding after the war. Overall, 51% of parenteral arsenicals used against yaws were administered IV. For bismuth salts,
Figure 12
shows the numbers of vials. However, most of the bismuth came as bulk powder, which was then diluted locally with water. For 1952–4, it can be calculated that some 500,000 additional injections of bismuth were made each year. In AEF-3, use of parenteral arsenicals doubled to 394,189 vials in 1949; there is little information about bismuth
. Mercury salts, cheaper but much more toxic, were abandoned in 1951
.
When penicillin became available, older drugs were not abandoned immediately because the supply of the revolutionary drug was limited (and one can imagine that African colonies were not at the top of the list). In 1957, of 91,032 syphilis cases in Cameroun, 6% were treated with IM penicillin alone; others received metallic drugs alone (72%) or in combination with penicillin (23%). For yaws (105,513 cases) corresponding proportions were 43%, 46% and 11%
.
.
It is remarkable that such a high incidence of yaws persisted despite millions of injections of metallic drugs, decreasing only after the introduction of penicillin, which was more effective, less toxic and easier to administer. The development of a depot form of penicillin, slowly absorbed from the muscle, made it possible to treat with a single IM injection the patients, their asymptomatic family contacts and, in some communities, all children
. This eventually interrupted the chain of transmission but the disease was never eradicated. When incidence of yaws dropped to a low level, control programmes were discontinued, as this intervention now seemed far too costly compared to its limited health impacts.
. This eventually interrupted the chain of transmission but the disease was never eradicated. When incidence of yaws dropped to a low level, control programmes were discontinued, as this intervention now seemed far too costly compared to its limited health impacts.
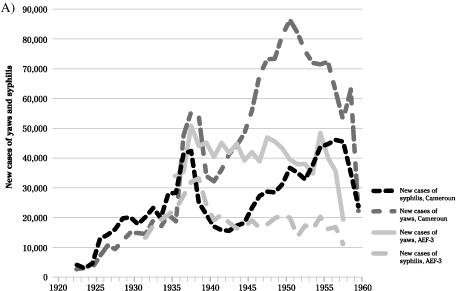
New cases of yaws and syphilis and consumption of antitreponemal drugs in Cameroun Français and AEF-3.
Adapted from Pepin.
10
10
Other books
Dalva by Jim Harrison
Project 17 by Laurie Faria Stolarz
56: Joe DiMaggio and the Last Magic Number in Sports by Kennedy, Kostya
Spellscribed: Ascension by Cruz, Kristopher
The Iron Grail by Robert Holdstock
The Mommy Mystery by Delores Fossen
My Mother's Body by Marge Piercy
Elizabeth and the Vampire's Cabin by Leilani Allmon
The Owl Killers by Karen Maitland
Fireborn Champion by AB Bradley