Vaccinated (5 page)
Authors: Paul A. Offit

Â
J
ENNER NEEDED COWS TO MAKE HIS SMALLPOX VACCINE;
P
ASTEUR
needed dogs and rabbits. From Alexis Carrel, Hilleman learned that animal organs could be kept alive outside of the body, freeing researchers from using whole animals when they wanted to make their vaccines.
On January 17, 1912âthree months before the steamship
Titanic
sank in the Atlantic OceanâCarrel, a French surgeon working at the Rockefeller Institute in New York City, removed a small piece of heart from an unhatched chick embryo and placed it in the bottom of a flask. Every two days he added nutrient fluid that contained chicken plasma and a crude extract made from a chicken embryo. He wanted to see how long he could keep the piece of chicken heart alive. Obsessed that the heart might be inadvertently contaminated with bacteria, Carrel created a cult around its maintenance, insisting that the walls be painted black and that his technicians wear long black gowns with hoods when they entered the room in which it was kept. To celebrate their success, every January doctors and nurses at the Rockefeller Institute lined up outside the research laboratory, locked hands, and joined Carrel in lustily singing ”Happy Birthday” to the small piece of heart. Carrel and his colleagues maintained the chicken heart fragment until his death in 1944.
Â
F
ROM
E
RNEST
G
OODPASTURE, WHO WORKED IN THE EARLY
1930s, H
ILLEMAN
learned that viruses could be grown in eggs, a discovery that forged a permanent bond between virologists and chicken farmers.
Born on a farm near Clarksville, Tennessee, Goodpasture, a quiet, unassuming pathologist, was interested in fowlpox, a virus similar to smallpox. Because fowlpox infected chickens, he decided to try to grow the virus in hens' eggs, reasoning that eggs were sterile (antibiotics hadn't been invented yet) and inexpensive. Working at Vanderbilt University in Nashville, Goodpasture took an incubating hen's egg, bathed it in alcohol, and, to sterilize the shell, set it on fire. Then, using an eggcup as an operating table, he cut a small window in the shell and injected the egg with fowlpox. The virus grew readily in the membrane surrounding the chick embryo. Hilleman used Goodpasture's technique to make his pandemic influenza and mumps vaccines.
Â
F
ROM
M
AX
T
HEILER
, H
ILLEMAN LEARNED THAT HUMAN VIRUSES COULD
be weakened and made into vaccines by growing them in animal cells. (Remember, Hilleman weakened his daughter's mumps virus by growing it in chick cells.)
Theiler, a South African émigré also working at the Rockefeller Institute, wanted to make a vaccine to prevent yellow fever, a tropical viral disease that caused bleeding, the unmistakable symptom of black vomit, jaundiceâa yellowing of the eyes and skin that gave the virus its nameâand death. Because yellow fever virus caused severe internal bleeding, it was called a viral hemorrhagic fever. Yellow fever was common in the United States; an outbreak in Philadelphia in the late 1700s killed 10 percent of the city's residents, and an outbreak in New Orleans in the mid-1800s killed 30 percent. The terror once caused by yellow fever is associated today with another viral hemorrhagic fever: Ebola virus.
In the mid-1930s, Max Theiler performed a series of experiments that determined how researchers would make viral vaccines for the next seventy years. Using Carrel's technique of growing chopped-up animal organs in laboratory flasks, Theiler found that yellow fever virus grew in mouse embryos. So he passed the virus from one mouse embryo to another and eventually from one chicken embryo to another. Theiler reasoned that as yellow fever virus got better and better at growing in cells from different speciesâlike mice and chickensâit would become less and less capable of causing disease in humans. (Today we know that human viruses forced to grow in animal cells undergo a series of genetic changes that make them less capable of reproducing and causing disease in people.) To test his theory, Theiler injected a thousand Brazilians with what he hoped was a weakened form of yellow fever virus. He found that most people developed antibodies to the virus and that no one got the disease. By the end of the 1930s, Theiler had inoculated more than half a million Brazilians, and epidemics of yellow fever in Brazil abated. The yellow fever vaccine made in mouse embryos by Max Theiler in the mid-1930s is still used today.
Theiler's technique of weakening human viruses by growing them in cells from other species remains the single most important method for making live weakened viral vaccines. His method has been used to make vaccines against measles, mumps, rubella, chickenpox, and polio. In 1951, “for his discoveries concerning yellow fever and how to contain it,” Max Theiler won the Nobel Prize in medicine. When asked what he planned to do with the $36,000 in prize money, he said “Buy a case of Scotch and watch the [Brooklyn] Dodgers.”
Like Jenner and Pasteur before him, Theiler also saw tragedy follow his vaccine. In the early 1940s, scientists made Theiler's vaccine using human serum obtained from several volunteers, to stabilize the virus. Unfortunately, unnoticed at the time, at least one of these volunteers was jaundiced, infected with hepatitis B virus. As a consequence, more than three hundred thousand American servicemen injected with contaminated yellow fever vaccine got hepatitis, and sixty died. Human serum was never again used to stabilize vaccines.
Â
F
ROM THE RESEARCH TEAM OF
J
OHN
E
NDERS
, T
HOMAS
W
ELLER, AND
Frederick Robbins, working at Boston Children's Hospital (part of Harvard's Medical School) in the late 1940s, Hilleman learned how to grow animal and human cells in the laboratory. Alexis Carrel's technique, using chopped up animal organs, was called tissue culture; the Enders group's technique, using single layers of animal or human cells grown in laboratory flasks, was called cell culture. Now when researchers want to grow viruses, they simply take a vial of cells out of the freezer, thaw them out, place them into laboratory flasks, watch them reproduce until a single layer neatly covers the bottom of the flask, and inoculate them with viruses. The days of growing viruses in whole animals or chopped-up animal organs were over. The Enders group's technique is still used to make viral vaccines today.
One of the Boston group's first cell cultures was made from a human fetus. On March 30, 1948, at 8:30 a.m., Thomas Weller walked across the street in front of Boston Children's Hospital and into the office of Duncan Reid, an obstetrician working at the Boston Lying-In Hospital who had just aborted a twelve-week pregnancy. The mother had chosen to end her pregnancy because she had been infected with rubella, a virus known to cause birth defects. Reid handed Weller the fetus. After coaxing fetal cells to reproduce on the bottom of laboratory flasks, Weller found that polio virus grew in the cells. Weller, Robbins, and Enders found later that polio virus also grew in a variety of different animal and human cells. Prior to these experiments, polio virus could be grown only in cells from brains and spinal cords. Researchers feared using a polio vaccine made from nervous tissue for the same reason that they feared Pasteur's vaccine: the dangerous side effect of autoimmunity.
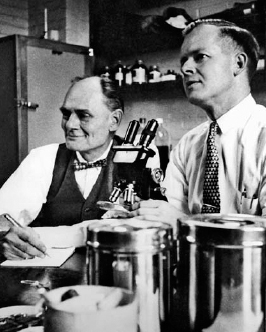
John Enders (left) and Thomas Weller in their laboratory at Boston Children's Hospital, November 1954 (courtesy of the March of Dimes Birth Defects Foundation).
In 1954 Enders, Weller, and Robbins won the Nobel Prize in medicine for “their discovery of the ability of polio viruses to grow in cultures of various types of tissue.” These studies allowed Jonas Salk and Albert Sabin to make polio vaccines that eventually eliminated polio from most of the world.
Â
F
ROM
J
ONAS
S
ALK, THE SCIENTIST WHO FIRST FOUND A WAY TO
prevent polio, Hilleman learned that vaccines could win the heart of the American public.
Born and raised in New York City, the son of Russian immigrants, Salk was driven, obstinate, and self-assured. Working at the University of Pittsburgh in the early 1950s, Salk used the Enders group's technique to grow polio virus in monkey kidney cells. Then he purified the virus, killed it with formaldehyde, and injected it into seven hundred children in and around Pittsburgh. Salk reasoned that killed polio virus would induce polio antibodies but wouldn't cause polio. In 1954, funded by the March of Dimes, doctors and nurses injected four hundred thousand children with Salk's vaccine and two hundred thousand with an inert liquid that looked like vaccine, called placebo. The program was then and remains today the largest test of a medical product ever performed. Following the announcement that the vaccine worked, Americans named hospitals, schools, streets, and babies after Salk and sent him money, clothes, and cars. Universities offered him honorary degrees, and countries issued proclamations in his honor. Salk started the day as a scientist at the University of Pittsburgh and ended it as one of the most revered men on the face of the earth. When people hear the word
vaccine
today, the first person they think of is Jonas Salk.
But like Jenner, Pasteur, and Theiler before him, Salk watched tragedy follow his vaccine. When Salk found that polio vaccine could be made by inactivating polio virus with formaldehyde, five companies stepped forward to make it. On April 12, 1955, each of those companies was permitted to sell its vaccine to the public. One company, Cutter Laboratories of Berkeley, California, made it badly. Researchers and executives at Cutter were confident that they had made their polio vaccine exactly as Jonas Salk had prescribed, giving it to the children of four hundred and fifty of their employees. But, because Cutter researchers hadn't properly filtered out the cells in which they grew polio virus, some virus particles had effectively escaped the killing effects of formaldehyde. As a consequence, more than one hundred thousand children were inadvertently injected with live, dangerous polio virus. Worse, children injected with Cutter's vaccine spread polio to others, starting the first and only man-made polio epidemic. When the dust settled, live polio virus contained in Cutter's vaccine had infected two hundred thousand people; caused about seventy thousand to have mild cases of polio; permanently and severely paralyzed two hundred people, mostly children; and killed ten. It was one of the worst biological disasters in American history. Federal regulators quickly identified the problem with Cutter's vaccine and established better standards for vaccine manufacture and safety testing. Cutter Laboratories never again made another polio vaccine. And Salk's polio vaccine helped to dramatically reduceâand in some countries eliminateâone of the world's most crippling infections.
Â
H
ILLEMAN HAD LEARNED FROM WHAT HAD GONE RIGHT AND WHAT
had gone wrong before him. By the time he made his mumps vaccine, an enormous path had been cleared through the thicket. “It was an age of genius,” he said. “I was able to do what I did because of what they did.”
4
The Destroying Angel
“That fatal and never to be forgotten year, 1759, when the Lord sent the destroying Angel to pass through this place, and removed many of our friends into eternity in a short space of time; and not a house exempt, not a family spared from the calamity. So dreadful was it that it made every ear tingle, and every heart bleed; in which time I and my family were exercised with that dreadful disorder, the measles. But by blessed God our lives were spared.”
E
PHRAIM
H
ARRIS, COLONIST AND FARMER,
F
AIRFIELD
, N
EW
J
ERSEY
W
hile Maurice Hilleman was making his mumps vaccine, he was also making a measles vaccine.
Measles infection starts innocently enough, with fever, cough, a runny nose, pinkeye, and rash. But measles virus also can infect the lungs, causing fatal pneumonia, and the brain, causing seizures, deafness, and permanent brain damage. And it can infect the liver, kidneys, heart, and eyes, blinding many survivors. Furthermore, measles virus causes one of the most insidious, unrelenting diseases of childhoodâsubacute sclerosing panencephalitis (SSPE), a rare but uniformly fatal disorder. Symptoms of SSPE usually begin about seven years after measles infection. At first children undergo subtle personality changes, their handwriting deteriorates, and they seem to forget things. Later, when the horror of the disease fully emerges, children are progressively less able to walk, stand, or talk; then they become combative, have seizures, lapse into a coma, and die. Despite decades of study, a parade of drugs, and heroic supportive measures, no child has ever survived SSPE.
In the early 1960s, when Maurice Hilleman wanted to make his vaccine, measles virus was killing eight million children in the world every year. Doctors and public health officials were desperate to find a way to prevent it.
Â
T
HE ROAD TO A MEASLES VACCINE STARTED IN
B
OSTON.
In 1954, Thomas Peebles was working in the laboratory of John Enders at Boston Children's Hospital. The team, which had just won the Nobel Prize in medicine for its work on polio, also included Sam Katz, a brilliant infectious diseases specialist and pediatrician from New Hampshire, and Milan Milovanovic, a scientist from Belgrade, Yugoslavia. Peebles, fresh from his internship at Massachusetts General Hospital, had gotten a late start in his career, spending four years in the navy during the Second World War. Enders assigned Peebles the task of capturing measles virus. Although researchers were sure that a virus caused measles, no one had ever coaxed it to reproduce inside a test tube.
In January 1954, Peebles got the break he was looking for. Dr. Theodore Ingalls called Peebles and told him about an outbreak of measles at the Fay School, an exclusive all-boys private school in Southborough, a suburb west of Boston. (The school, founded in 1866, was one of the oldest boarding schools in the United States.) Peebles got into his car, drove thirty miles, and convinced the school's principal, Harrison Reinke, to allow him to collect blood from the boys. Then he went to each student and said, “Young man, you are standing on the frontiers of science. We are trying to grow this virus for the first time. If we do, your name will go into our scientific report of the discovery. Now this will hurt a little. Are you game?”
For the next few weeks Peebles tried unsuccessfully to capture measles virus. But on February 8, 1954, his luck changed. David Edmonston, a thirteen-year-old student at Fay, had stomach cramps, nausea, fever, and a faint red rash that started on his face and spread to his chest, abdomen, and back. When David's temperature rose to 104 degrees, large quantities of measles virus coursed through his veins. Thomas Peebles was about to do something that no one had dared to do before: make a vaccine using human organs.
In the early 1950s, doctors subjected children to a medical procedure, now abandoned, for a condition called hydrocephalusâliterally, “water on the brain.” In the center of the brain, specialized cells make fluid that bathes the spinal cord; the fluid must travel through a series of narrow canals. Sometimes, because of infection or birth defects, those canals are blocked and spinal fluid is trapped, compressing the brain. To relieve the blockage, surgeons would drill a small hole into the center of the brain, insert a plastic catheter, and create a tunnel under the skin that ended in the ureter, a tube that connects the kidneys to the bladder. In order to connect the catheter to the ureter, surgeons needed to remove a kidneyâone perfectly healthy, fully functioning human kidney. Now, instead of spinal fluid getting trapped in the brain, it was carried to the bladder and urinated out of the body.
Enders couldn't bear to see healthy kidneys wasted. “He was the typical penurious Yankee,” recalled Sam Katz. “He just hated to see things wasted. And his thriftiness extended to [laboratory] materials.” So Enders sent Thomas Peebles to collect the kidneys before they were thrown away and asked him to try to grow measles virus in them. First, Peebles treated the kidneys with a powerful enzyme to make sure the kidney cells didn't clump together. Then he put the cells into sterile flasks, watched them reproduce until they covered the bottom of each flask, and added David Edmonston's blood. After a few days, the kidney cells shriveled up and died. Edmonston's measles virus was apparently reproducing inside the cells, killing them in the process.
Now that the Boston researchers could grow measles virus in laboratory cells, they could weaken it to make a vaccine. Peebles, Katz, and Milovanovic grew the virus serially in twenty-four cultures of human kidneys, twenty-eight cultures of human placentas (Enders apparently couldn't stand to watch placentas getting thrown away either), six hens' eggs, and six minced chick embryos. They hoped that by forcing David Edmonston's measles virus to grow in this hodgepodge of human and animal cells, the virus would weaken sufficiently to be a vaccine. There was, however, no formula, no recipe, for how to do this.
Thomas Weller remembered what it was like to work in a laboratory dense with human kidneys and placentas: “I would walk across the street to the Boston Lying-In Hospital, and obstetricians would hand me these heavy placentas from babies that they'd just delivered. Some days there were no placentas. But on others there were as many as six. Back in Dr. Enders's laboratory I set up two ring stands and balanced a thick, sterile steel rod between them. Then I draped the placentas over the rods like clothes on a clothesline.”
Â
N
OW IT WAS TIME FOR THE
B
OSTON TEAM TO TEST THE VACCINE. SO
Sam Katz drove to the Fernald School, where a few years earlier researchers had fed radioactive cereal to members of its science club. “We chose the Fernald School because every year there were outbreaks of measles [in the school],” recalled Katz, “and every year several children died.” On October 15, 1958, Katz injected eleven mentally retarded or disabled children with the vaccine developed in Enders's laboratory. All the children developed protective antibodies. But eight of them had fever, and nine had a mild rash. Although the vaccine protected children from measles without causing the full-blown disease, the vaccine still wasn't weak enough.
Without weakening the virus further, the Boston team next tested the vaccine in mentally retarded children at the Willowbrook State School, where Saul Krugman had performed his controversial experiments with hepatitis virus. On February 8, 1960, Katz injected twenty-three children with the vaccine, and twenty-three other children were given nothing. Six weeks later an outbreak of measles swept through Willowbrook, infecting hundreds of children and killing four. None of the vaccinated children got measles, but many unvaccinated children did. Enders's vaccine worked but, again, had caused a high rate of side effects. “[Representatives from] many pharmaceutical companies came and got material to produce vaccines,” recalled Katz. “One was Maurice Hilleman.”
Â
H
ILLEMAN WAS EXCITED ABOUT WORKING WITH THE VACCINE DEVELOPED
by the Boston group. But he faced two difficult problems. Neither was easily solved.
The first involved side effects. Although the Enders team had passed David Edmonston's measles virus through several different human and animal cells, the virus still wasn't weak enough. Hilleman found, in experiments involving hundreds of healthy children, that half of those given Enders's vaccine had a rash, and most had fevers, some higher than 103 degrees. “It was toxic as hell,” recalled Hilleman. “Some children had fevers so high that they had seizures. The Enders strain was the closest thing there was to a vaccine, but to me it was just an isolate. He hadn't made a vaccine.” Even while he was worried about the safety of Enders's vaccine, Hilleman felt pressured by public health agencies anxious to prevent a disease that was killing thousands of American children every year. He had to find a way to make Enders's vaccine safer, and he had to do it quickly. The toxic-as-hell problem was solved by Joseph Stokes Jr., the pediatrician who had helped Hilleman test his mumps vaccine.
Hilleman chose Stokes because he was an expert on gamma globulin, the fraction of blood that contains antibodies. To make gamma globulin, Stokes took blood, let it clot, and stored it in the refrigerator. Eventually, red blood cells formed a clot at the bottom of the tube, and gamma globulin, contained in serum, floated to the top. Stokes knew that people infected with measles, mumps, polio, or hepatitis viruses rarely got the disease again. And he knew that antibodies were the reason why. In the mid-1930s, Stokes showed that gamma globulin taken from polio survivors protected children during polio epidemics. Ten years later, as a special consultant to the surgeon general during the Second World War, Stokes showed that gamma globulin from hepatitis survivors protected American soldiers from hepatitis. For his work on hepatitis, Stokes won the Presidential Medal of Freedom, the nation's highest civilian award.
Stokes proposed giving a tiny dose of gamma globulin along with Enders's measles vaccine, hoping to modify side effects. To see if the idea worked, Stokes and Hilleman went to a women's prison in central New Jersey.
Â
B
UILT IN
1913
ON A SPRAWLING FARM IN RURAL
H
UNTINGTON
C
OUNTY,
Clinton Farms for Women was an ideal prison. An outgrowth of the turn-of-the-century prison reform movement, Clinton provided education, technical training, medical care, and a safe environment for inmates. In the early 1960s, Hilleman and Stokes made several visits to Clinton Farms. (During one early visit, they were eating lunch in the cafeteria when a waitress came to the table and asked them what they wanted to eat. Hilleman needed the prisoners to feel comfortable with his experiment, and he knew that the waitress was also a prisoner. “So what are you in for?” he asked, awkwardly, trying to make conversation. “I killed my parents,” she replied. Seeing the stricken look on his face, she added, “But don't worry. You're safe here.” Hilleman never asked that question again and, despite her assurances, never felt completely safe on subsequent visits.)
Edna Mahan, the prison's director, revolutionized life at Clinton Farms by taking the locks off doors and prohibiting guards from carrying guns. Prisoners could walk off the grounds any time they wanted. “The prisoners would leave the prison, travel down the road, get into a passing truck, and get themselves pregnant,” recalled Hilleman. “The nursery was full of babies.”
Stokes and Hilleman injected six infants with Enders's vaccine in one arm and gamma globulin in the other. None of the infants had a high fever, and only one had a mild rash. Encouraged, they tested hundreds of children. In the end, Stokes's gamma globulin strategy worked. Subsequent studies during the next few years showed that the percentage of children with rash decreased from 50 percent to 1, and with fever from 85 percent to 5.
Edna Mahan died in 1968, only a few years after Hilleman performed studies in her prison's nursery. In a small cemetery on the prison grounds, her elaborate tombstone is surrounded by forty tiny crosses, each representing babies who died in the prison from infections that are now easily prevented by vaccines.
Â
T
HE SECOND PROBLEM THAT WORRIED
H
ILLEMAN WAS THAT ENDERS'S
vaccine might cause cancer. Although measles virus didn't cause cancer, Hilleman had reason to be concerned. His fears stemmed from an event that had occurred fifty years earlier.
In 1909 a farmer walked into the Rockefeller Institute in New York City carrying a dead chicken under his arm. Hands thickened by hard work, wearing thick bib overalls and heavy boots, the farmer watched as scientists, technicians, and graduate students milled through the lobby of one of the country's premier research institutes. Finally he got up the courage to ask where he could find Peyton Rous's laboratory. The farmer was certain that Rous, an expert in animal diseases, would know what had happened to his chicken.
A Baltimore-bred, Johns Hopkinsâtrained pathologist, Peyton Rous was thirty years old when he took the chicken from the farmer, laid it onto his laboratory bench, and dissected it. Just under the right breast was a large cancerous tumor. Rous found that the cancer had also spread to the liver, lungs, and heart. He asked the farmer whether any other chickens in his flock had a similar problem. “No,” the farmer said, “only this one.” Apparently, the cancer wasn't contagious.
Rous wanted to find what had caused the chicken's cancer. So he removed the tumor and carefully ground it up with sterile sand, completely destroying all the malignant tumor cells. Then he suspended the disrupted tumor cells in salt water and passed them through unglazed porcelain, which acted as a filter to trap bacteria. Rous found that when he injected the fluid that had passed through the filter into other chickens, tumors developed in those chickens as well. Within a few weeks, cancer had killed them all. “The [chickens] became emaciated, cold, and drowsy, and shortly died,” he said. Because the tumors were caused by something passing through the filters, Rous knew that it couldn't be bacteria. And he knew that it couldn't be the cancer cells, because they had been destroyed by the sand and were too big to pass through the filters. It was something else. Rous reasoned that the agent that had passed through the filters was a virus.
On January 11, 1911, Peyton Rous, in a paper titled “Transmission of a Malignant Growth by Means of a Cell-Free Filtrate,” was the first person to prove that viruses could cause cancer. Immediately other investigators tried to duplicate Rous's findings in mice and rats, but without success. Reasoning that cancer-causing viruses were at most a phenomenon unique to chickens, Rous gave up his investigations in 1915, and for the next four decades researchers relegated tumor viruses to the cabinet of freaks.