Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine (7 page)
Read Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine Online
Authors: Marc Sabatine
Tags: #Medical, #Internal Medicine

BOOK: Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine
11.08Mb size Format: txt, pdf, ePub
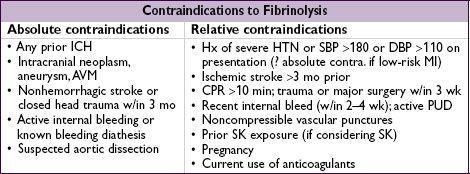
Fibrinolysis
• Indic: STE/LBBB + sx <12 h; benefit if sx >12 h less clear; reasonable if persist. sx & STE
• Mortality ↓
20% in anterior MI or LBBB and
10% in IMI c/w reperfusion Rx • Prehospital lysis (ie, ambulance): further 17% ↓ in mortality (
JAMA
2000;283:2686) •
1% risk of ICH; high-risk groups include elderly (
2% if >75 y), women, low wt • Although age not contraindic., ↑ risk of ICH in elderly (>75 y) makes PCI more attractive
Nonprimary PCI
• Facilitated PCI: upstream lytic, GPI or GPI + ½ dose lytic before PCI offers no benefit • Rescue PCI if shock, unstable, failed reperfusion or persistent sx (
NEJM
2005;353:2758) • Routine angio ± PCI w/in 24 h of successful lysis: ↓ D/MI/revasc (
Lancet
2004;364:1045) and w/in 6 h ↓ reMI, recurrent ischemia, & HF compared to w/in 2 wk (
NEJM
2009;360:2705);
∴
if lysed at non-PCI capable hospital, consider transfer to PCI-capable hospital ASAP esp. if high-risk presentation (eg, anterior MI, inferior MI w/ low EF or RV infarct, extensive STE or LBBB, HF
, ↓
BP or
↑
HR
)
•
Late
PCI (median day 8) of occluded infarct-related artery: no benefit (
NEJM
2006;355:2395)
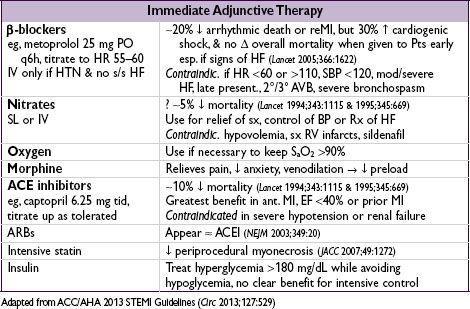
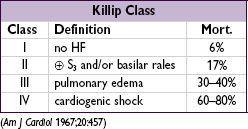
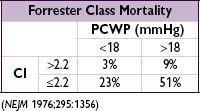
LV failure (~25%)
• Diurese to achieve PCWP 15–20 → ↓ pulmonary edema, ↓ myocardial O
2
demand • ↓ Afterload → ↑ stroke volume & CO, ↓ myocardial O
2
demand
can use IV NTG or nitroprusside (risk of coronary steal) → short-acting ACEI
• Inotropes if HF despite diuresis & ↓ afterload; use dopamine, dobutamine or milrinone •
Cardiogenic shock
(~7%) = MAP <60 mmHg, CI <2 L/min/m
2
, PCWP >18 mmHg; inotropes, mech support [eg, VAD, IABP (trial w/o benefit
NEJM
2012;367:1287)] to keep CI >2; pressors to keep MAP >60; if not done already, coronary revasc (
NEJM
1999;341:625)
IMI complications (
Circ
1990;81:401;
NEJM
1994;330:1211;
JACC
2003;41:1273)
•
Heart block
(~20%, occurs because RCA typically supplies AV node)
40% on present., 20% w/in 24 h, rest by 72 h; high-grade AVB can develop abruptly
Rx: atropine, epi, aminophylline (100 mg/min × 2.5 min), temp wire
•
RV infarct
(30–50%, but only ½ of those clinically signif). HoTN; ↑ JVP,Kussmaul’s; 1 mm STE in V
4
R; RA/PCWP ≥0.8; RV dysfxn on TTE; prox RCA occl.
Rx: optimize preload (RA goal 10–14,
BHJ
1990;63:98); ↑ contractility (dobutamine); maintain AV synchrony (pacing as necessary); reperfusion (
NEJM
1998;338:933); mechanical support (IABP or RVAD); pulmonary vasodilators (eg, inhaled NO)
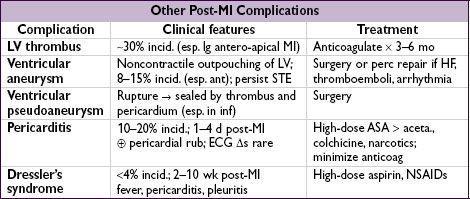
Mechanical complications (incid. <1% for each; typically occur a few days post-MI)
•
Free wall rupture
: ↑ risk w/ lysis, large MI, ↑ age,, HTN; p/w PEA or hypoTN, pericardial sx, tamponade; Rx: volume resusc., ? pericardiocentesis, inotropes,
surgery
•
VSD
: large MI in elderly; AMI → apical VSD, IMI → basal septum; 90% w/ harsh murmur ±
thrill (
NEJM
2002;347:1426); Rx: diuretics, vasodil., inotropes, IABP,
surgery
, perc. closure
•
Papillary muscle rupture
: more common after inf MI (PM pap. muscle supplied by PDA alone) than ant MI (AL pap. muscle supplied by diags & OMs); 50% w/ new murmur, rarely a thrill, ↑
v
wave in PCWP tracing; asymmetric pulmonary edema. Rx: diuretics, vasodilators, IABP,
surgery
.
Arrhythmias post-MI
• Treat as per ACLS for unstable or symptomatic bradycardias & tachycardias •
AF
(10–16% incidence): β-blocker or amio, ± digoxin (particularly if HF), heparin •
VT/VF
: lido or amio × 6–24 h, then reassess; ↑ βB as tol., replete K & Mg, r/o ischemia;
early monomorphic (<48 h post-MI) does
not
carry bad prognosis
• Accelerated idioventricular rhythm (AIVR): slow VT (<100 bpm), often seen after
successful reperfusion; typically self-terminates and does not require treatment
• May consider
backup
transcutaneous pacing
(TP) if: 2° AVB type I, BBB
•
Backup TP
or
initiate transvenous pacing
if: 2° AVB type II; BBB + AVB
•
Transvenous pacing
(TV) if: 3° AVB; new BBB + 2° AVB type II; alternating LBBB/RBBB (can bridge w/ TP until TV, which is best accomplished under fluoroscopic guidance)
Prognosis
• In registries, in-hospital mortality is 6% w/ reperfusion Rx (lytic or PCI) and ~20% w/o • Predictors of mortality: age, time to Rx, anterior MI or LBBB, heart failure (
Circ
2000;102:2031)
Other books
Tree of Life and Death by Gin Jones
The Union by Robinson, Gina
A Wicked Snow by Gregg Olsen
Everyday Paleo by Sarah Fragoso
The Siege of White Deer Park by Colin Dann
Who Owns the Future? by Jaron Lanier
Among the Ten Thousand Things by Julia Pierpont
Dragon Warrior (Midnight Bay) by Janet Chapman
Just Joshua by Jan Michael
Take (Need #2) by K.I. Lynn, N. Isabelle Blanco