Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine (6 page)
Read Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine Online
Authors: Marc Sabatine
Tags: #Medical, #Internal Medicine

BOOK: Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine
3.3Mb size Format: txt, pdf, ePub
•
Cardiac biomarkers
(Tn preferred, or CK-MB): ✓ Tn at baseline & 3–6 h after sx onset; a rise to >99th %ile in approp. clinical setting dx of MI (see “Chest Pain”); nb, in Pts w/ ACS & ↓ CrCl, ↑ Tn still portends poor prognosis (
NEJM
2002;346:2047) • If low prob,
stress test
,
CT angio
or rest perfusion imaging to r/o CAD (see “Chest Pain”) • TTE (new wall motion abnl) suggestive of ACS; coronary angio gold standard for CAD
Prinzmetal’s (variant) angina
• Coronary spasm → transient STE usually w/o MI (
but
MI, AVB, VT can occur) • Pts usually young, smokers, ± other vasospastic disorders (eg, migraines, Raynaud’s) • Angiography → nonobstructive CAD, focal spasm w/ hyperventilation, acetylcholine • Treatment: high-dose CCB, nitrates (+SL NTG prn), ? a-blockers; d/c smoking • Cocaine-induced vasospasm: use CCB, nitrates, ASA; ? avoid bB, but data weak and labetalol appears safe (
Archives
2010;170:874;
Circ
2011;123:2022)
Approach to triage
• If hx and initial ECG & biomarkers non-dx, repeat ECG & biomarkers 3–6 h later • If remain nl and low likelihood of ACS, search for alternative causes of chest pain • If remain nl, have ruled out MI,
but
if suspicion for ACS based on hx, then still need to r/o UA w/ stress test to assess for inducible ischemia (or CTA to r/o CAD);
if low risk (age ≤70; prior CAD, CVD, PAD; rest angina) can do as outPt w/in 72 h (0% mortality, <0.5% MI,
Ann Emerg Med
2006;47:427)
if not low risk, admit and initiate Rx for possible ACS and consider stress test or cath
Coronary angiography (
Circ
2007;116:e148 & 2012;126:875)
•
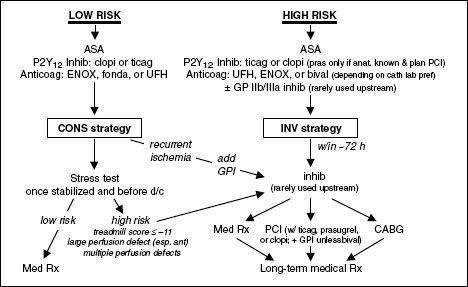
Conservative strategy
= selective angiography. Medical Rx with pre-d/c stress test; angio only if recurrent ischemia or stronglyETT.
Indicated for
: low TIMI risk score, Pt or physician preference in absence of high-risk features, low-risk women (
JAMA
2008;300:71).
•
Invasive strategy
= routine angiography w/in 72 h
Immediate (w/in 2 h) if
: refractory/recurrent ischemia, hemodynamic or electrical instability
Early (w/in 24 h) if
:Tn, ST Δ, TRS ≥3, GRACE risk score >140 (
NEJM
2009;360:2165)
Delayed (ie, acceptable anytime w/in 72 h) if
: diabetes, EF <40%, GFR <60, post-MI angina, PCI w/in 6 mo, prior CABG or high-risk stress results
32% ↓ rehosp for ACS, nonsignif 16% ↓ MI, no Δ in mortality c/w cons. (
JAMA
2008;300:71)
↑ peri-PCI MI counterbalanced by ↓↓ in spont. MI
Mortality benefit seen in some studies, likely only if cons. strategy w/ low rate of angio
Figure 1-2
Approach to UA/NSTEMI
STEMI
Requisite STE (at J point)
• ≥2 contiguous leads w/ ≥1 mm (except for V
2
–V
3
: ≥2 mm inand ≥1.5 mm in
) • New or presumed new LBBB
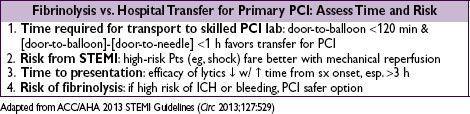
Reperfusion (“time is muscle”)
• Immediate reperfusion (ie, opening occluded culprit coronary artery) is critical • In PCI-capable hospital, goal should be
primary PCI
w/in 90 min of 1st medical contact • In non-PCI-capable hospital, consider
transfer
to PCI-capable hospital (see below), o/w
fibrinolytic therapy
w/in 30 min of hospital presentation • Do not let decision regarding
method
of reperfusion delay
time
to reperfusion
Primary PCI (
NEJM
2007;356:47)
• Indic: STE + sx <12 h; ongoing ischemia 12–24 h after sx onset; shock regardless of time • Superior to lysis: 27% ↓ death, 65% ↓ reMI, 54% ↓ stroke, 95% ↓ ICH (
Lancet
2003;361:13) • Thrombus aspiration during angio prior to stenting ↓ mortality (
Lancet
2008;371:1915) • Do not intervene on nonculprit lesions; risk stratify w/ imaging stress (
Circ
2011;124:e574) •
Transfer
to center for 1° PCI may also be superior to lysis (
NEJM
2003;349:733), see below
Other books
Leaving by Karen Kingsbury
Written in the Stars by LuAnn McLane
Peaches for Monsieur Le Curé by Joanne Harris
Billy and the Birdfrogs by B.B. Wurge
Mirrored Time (A Time Archivist Novel Book 1) by J.D. Faulkner
Hunting the Hero by Heather Boyd
Frogspell by C. J. Busby
The Other Side of Perfect by Victoria Peters
Emmy and the Rats in the Belfry by Lynne Jonell
The Gangbang Collection by Electra, Jane, Kane, Carla, De la Cruz, Crystal