The Origins of AIDS (5 page)
Read The Origins of AIDS Online
Authors: Pepin

Prevalence of SIV
cpz
among wild populations of
P.t. troglodytes
was then measured in an extraordinary study performed in ten forest sites throughout southern Cameroon. To make sure that the faeces originated from
P.t. troglodytes
and to avoid counting stools from any individual chimp more than once, the researchers amplified a number of host DNA sequences for species, gender and individual identification. In other words, they used the chimpanzee cells present in stools to fingerprint molecularly each and every individual ape who had defecated. After excluding degraded specimens, those that contained
gorilla (the trackers’ noses may not always be perfect!) or
P.t. ellioti
DNA, specimens were available from 106 individual
P.t. troglodytes
chimpanzees. Sixteen were infected with SIV
cpz
. Again, there was a lot of variation in SIV
cpz
prevalence between the study sites: in four of them not a single infection was found; in three sites prevalence was over 20% and the highest was 35%.
25
cpz
among wild populations of
P.t. troglodytes
was then measured in an extraordinary study performed in ten forest sites throughout southern Cameroon. To make sure that the faeces originated from
P.t. troglodytes
and to avoid counting stools from any individual chimp more than once, the researchers amplified a number of host DNA sequences for species, gender and individual identification. In other words, they used the chimpanzee cells present in stools to fingerprint molecularly each and every individual ape who had defecated. After excluding degraded specimens, those that contained
gorilla (the trackers’ noses may not always be perfect!) or
P.t. ellioti
DNA, specimens were available from 106 individual
P.t. troglodytes
chimpanzees. Sixteen were infected with SIV
cpz
. Again, there was a lot of variation in SIV
cpz
prevalence between the study sites: in four of them not a single infection was found; in three sites prevalence was over 20% and the highest was 35%.
25
Phylogenetic analyses (
Figure 3
) showed that all sixteen new SIV
cpz
isolates were closely related to SIV
cpz
isolates from captive
P.t. troglodytes
chimps and to HIV-1 groups M and N, but not to HIV-1 group O (always the outlier) or SIV
cpz
obtained from
P.t. schweinfurthii
.
This phylogenetic proximity confirmed – now irrefutably – that the SIV
cpz
of
P.t. troglodytes
of central Africa was indeed the source of HIV-1 group M. Game over for this part of the story.
Figure 3
) showed that all sixteen new SIV
cpz
isolates were closely related to SIV
cpz
isolates from captive
P.t. troglodytes
chimps and to HIV-1 groups M and N, but not to HIV-1 group O (always the outlier) or SIV
cpz
obtained from
P.t. schweinfurthii
.
This phylogenetic proximity confirmed – now irrefutably – that the SIV
cpz
of
P.t. troglodytes
of central Africa was indeed the source of HIV-1 group M. Game over for this part of the story.
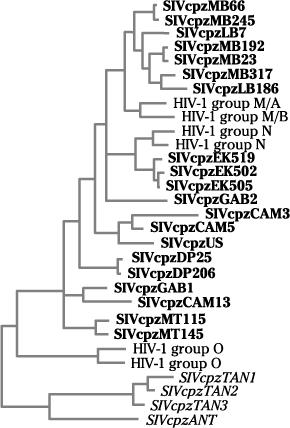
Figure 3
Phylogenetic analysis showing the relationship between SIV
cpz
from
P.t. troglodytes
chimpanzees in Cameroon or Gabon (bold) and isolates from humans infected with HIV-1 group M, HIV-1 group N and HIV-1 group O. SIV
cpz
isolates obtained from
P.t. troglodytes
cluster with the HIV-1 group M and N isolates, while HIV-1 group O remains an outlier. SIV
cpz
obtained from
P.t. schweinfurthii
chimpanzees in Tanzania or DRC (italics) lie further away.
Phylogenetic analysis showing the relationship between SIV
cpz
from
P.t. troglodytes
chimpanzees in Cameroon or Gabon (bold) and isolates from humans infected with HIV-1 group M, HIV-1 group N and HIV-1 group O. SIV
cpz
isolates obtained from
P.t. troglodytes
cluster with the HIV-1 group M and N isolates, while HIV-1 group O remains an outlier. SIV
cpz
obtained from
P.t. schweinfurthii
chimpanzees in Tanzania or DRC (italics) lie further away.
Adapted from Keele.
25
25
Chimpanzee populations separated by long distances or natural barriers like rivers harboured distinct lineages while adjacent troops harboured viruses closely related to each other. More detailed analyses of the genome showed strong clustering of human HIV-1 groups M and N viruses with the SIV
cpz
lineages obtained from some specific
P.t. troglodytes
troops in southern Cameroon. In other words, in these rural communities, the local strains of HIV-1 infecting humans genetically resembled the local strains of SIV
cpz
from the chimpanzees living close by. The SIV
cpz
isolates from south-east Cameroon, towards the border with Congo-Brazzaville and the
Central African Republic, were most closely related to
HIV-1 group M, while those from south-central Cameroon were closer to HIV-1 group N.
30
cpz
lineages obtained from some specific
P.t. troglodytes
troops in southern Cameroon. In other words, in these rural communities, the local strains of HIV-1 infecting humans genetically resembled the local strains of SIV
cpz
from the chimpanzees living close by. The SIV
cpz
isolates from south-east Cameroon, towards the border with Congo-Brazzaville and the
Central African Republic, were most closely related to
HIV-1 group M, while those from south-central Cameroon were closer to HIV-1 group N.
30
Additional faecal samples from
P.t. troglodytes
were collected over the following years, mostly in Cameroon, where the prevalence of SIV
cpz
infection is now estimated to be 5.9%, a figure that I will use for calculations in forthcoming chapters. In the
Central African Republic, no SIV
cpz
infection was found but fewer than fifty specimens have been tested
.
31
P.t. troglodytes
were collected over the following years, mostly in Cameroon, where the prevalence of SIV
cpz
infection is now estimated to be 5.9%, a figure that I will use for calculations in forthcoming chapters. In the
Central African Republic, no SIV
cpz
infection was found but fewer than fifty specimens have been tested
.
31
SIV infection was found among faeces from western gorillas (
Gorilla gorilla gorilla
); a virus which was called SIV
gor.
SIV
gor
is very similar to HIV-1 group O, rather than to group M. Thus gorillas are not the source of the HIV-1 group M pandemic
. Without getting into the details, chimpanzees may be the source of HIV-1 group O as well, which they transmitted to humans and to gorillas independently, or to gorillas first, which then infected some humans
.
31
–
33
Gorilla gorilla gorilla
); a virus which was called SIV
gor.
SIV
gor
is very similar to HIV-1 group O, rather than to group M. Thus gorillas are not the source of the HIV-1 group M pandemic
. Without getting into the details, chimpanzees may be the source of HIV-1 group O as well, which they transmitted to humans and to gorillas independently, or to gorillas first, which then infected some humans
.
31
–
33
Until proven otherwise, it is most likely that the modes of transmission of SIV
cpz
between chimpanzees are the same as in humans: sexual intercourse, from mother to child and possibly through blood–blood contacts. There is much sexual promiscuity in chimpanzees. For instance, one adult male in
Gombe is known to have mated since puberty at least 333 times with 25 different females, and of course only a very small proportion of all matings can be observed. A female called Flo was once observed to copulate fifty times within a twenty-four-hour period. The substantial genital swelling of females during oestrus may facilitate transmission of viruses by making the mucosa more fragile. Most of this sexual activity takes place within the closely knit community. A study of paternity among chimpanzee communities showed that only 7% of offspring had a father from outside the troop. Transmission
between troops could occur via out-migration of adolescent females, or during fights between males when blood-borne viruses could be exchanged
.
3
,
11
,
12
cpz
between chimpanzees are the same as in humans: sexual intercourse, from mother to child and possibly through blood–blood contacts. There is much sexual promiscuity in chimpanzees. For instance, one adult male in
Gombe is known to have mated since puberty at least 333 times with 25 different females, and of course only a very small proportion of all matings can be observed. A female called Flo was once observed to copulate fifty times within a twenty-four-hour period. The substantial genital swelling of females during oestrus may facilitate transmission of viruses by making the mucosa more fragile. Most of this sexual activity takes place within the closely knit community. A study of paternity among chimpanzee communities showed that only 7% of offspring had a father from outside the troop. Transmission
between troops could occur via out-migration of adolescent females, or during fights between males when blood-borne viruses could be exchanged
.
3
,
11
,
12
A weakness in the investigations of SIV among chimpanzees is the dearth of virological information about the fourth ape, the
Pan paniscus
bonobo. Previously called the pygmy chimpanzee, this was a misnomer since the difference in size compared to
Pan troglodytes
is minor. It inhabits parts of the DRC south of the
Congo but north of the
Kasaï–Sankuru river system, in the Congo central basin which has low human populations but is linked by rivers to Léopoldville–
Kinshasa, the main market for its farming and fishing products.
Pan paniscus
bonobo. Previously called the pygmy chimpanzee, this was a misnomer since the difference in size compared to
Pan troglodytes
is minor. It inhabits parts of the DRC south of the
Congo but north of the
Kasaï–Sankuru river system, in the Congo central basin which has low human populations but is linked by rivers to Léopoldville–
Kinshasa, the main market for its farming and fishing products.
Bonobos are less aggressive and more mutually tolerant than
P.t. troglodytes
, and males and females have similar social ranks (some primatologists even describe an unusual situation of female dominance). Bonobos are not territorial so that males do not stalk or attack males from other troops and interactions with other communities are generally peaceful. They have a particularly intense, peculiar – and dare I say – quasi-human sexual activity: they do it for fun rather than just for reproductive purposes, and they have sex mostly in what biologists call a ‘ventral–ventral mount’ (the ‘missionary position’). Among other practices that have been described by highly dedicated primatologists, they practise mutual genital–genital rubbing, genital massages, mouth kisses and even oral sex. Another unique feature of bonobos is their bisexuality, seen in both males and females.
34
–
36
P.t. troglodytes
, and males and females have similar social ranks (some primatologists even describe an unusual situation of female dominance). Bonobos are not territorial so that males do not stalk or attack males from other troops and interactions with other communities are generally peaceful. They have a particularly intense, peculiar – and dare I say – quasi-human sexual activity: they do it for fun rather than just for reproductive purposes, and they have sex mostly in what biologists call a ‘ventral–ventral mount’ (the ‘missionary position’). Among other practices that have been described by highly dedicated primatologists, they practise mutual genital–genital rubbing, genital massages, mouth kisses and even oral sex. Another unique feature of bonobos is their bisexuality, seen in both males and females.
34
–
36
About half of intercourses are preceded by some form of courtship, but once they copulate fifteen seconds suffice. Intercourse is used to solve conflicts and maintain social interactions, and female bonobos are known to accept sex in exchange for food, a process quite similar to some human behaviour that we shall describe later. The period of sexual receptivity of female bonobos is twice as long as for
Pan troglodytes
and bonobos are more likely to have promiscuous matings outside their own group. In principle, these factors could facilitate the sexual transmission of viruses.
Pan troglodytes
and bonobos are more likely to have promiscuous matings outside their own group. In principle, these factors could facilitate the sexual transmission of viruses.
Until recently only thirty-two bonobos, all but four living in zoos or primate centres in Europe and the US, had been tested for SIV
cpz
infection and none was infected. The main problem in studying
bonobos in the wild is that they are close to extinction, with between 10,000 and 20,000 individuals scattered around a large area of the DRC. Their distribution is discontinuous and bonobos are well aware that their main predator is humans. Just last year, samples from around sixty wild-living bonobos, obtained from two sites in the DRC, have finally been tested and were all negative for SIV. Given the heterogeneity in the distribution of SIV among
Pan troglodytes
, one would like a larger number of
Pan paniscus
troops to be tested, but in the meantime it is fair to say that there is no evidence that this primate played a role in the emergence of
HIV-1
.
28
,
37
–
38
cpz
infection and none was infected. The main problem in studying
bonobos in the wild is that they are close to extinction, with between 10,000 and 20,000 individuals scattered around a large area of the DRC. Their distribution is discontinuous and bonobos are well aware that their main predator is humans. Just last year, samples from around sixty wild-living bonobos, obtained from two sites in the DRC, have finally been tested and were all negative for SIV. Given the heterogeneity in the distribution of SIV among
Pan troglodytes
, one would like a larger number of
Pan paniscus
troops to be tested, but in the meantime it is fair to say that there is no evidence that this primate played a role in the emergence of
HIV-1
.
28
,
37
–
38
What was the source of SIV
cpz
infection in chimpanzees lies outside the scope of this book, which is to understand the early twentieth-century events that led to the current HIV-1 pandemic. To finish the story quickly, I will just add that, as reviewed elsewhere, SIV
cpz
probably originated from the recombination of distinct SIVs infecting smaller monkeys, principally the SIV
rcm
of red-capped mangabeys and a SIV which seems to infect greater spot-nosed monkeys, moustached guenons and mona monkeys. The most likely opportunity for such a recombination occurred when chimpanzees hunted and ate smaller monkeys. Perhaps the two SIVs that gave rise to SIV
cpz
were transmitted independently to different chimpanzees and spread for some time before an ape became infected with both, allowing recombination to occur. Alternatively, one of the SIVs could have established itself within the chimpanzee population, the recombination occurring when one of the chimps infected with the original SIV acquired a second SIV from a small monkey, again via predation
.
25
–
27
,
39
cpz
infection in chimpanzees lies outside the scope of this book, which is to understand the early twentieth-century events that led to the current HIV-1 pandemic. To finish the story quickly, I will just add that, as reviewed elsewhere, SIV
cpz
probably originated from the recombination of distinct SIVs infecting smaller monkeys, principally the SIV
rcm
of red-capped mangabeys and a SIV which seems to infect greater spot-nosed monkeys, moustached guenons and mona monkeys. The most likely opportunity for such a recombination occurred when chimpanzees hunted and ate smaller monkeys. Perhaps the two SIVs that gave rise to SIV
cpz
were transmitted independently to different chimpanzees and spread for some time before an ape became infected with both, allowing recombination to occur. Alternatively, one of the SIVs could have established itself within the chimpanzee population, the recombination occurring when one of the chimps infected with the original SIV acquired a second SIV from a small monkey, again via predation
.
25
–
27
,
39
3
The timing
A colonial tragedy
Instructive autopsies
The timing
Having identified the source of HIV-1, the next question is:
when
did the virus manage to cross species from chimps to humans? It has often been said that AIDS was a new disease on the African continent. Apart from the published cases mentioned in
Chapter 1
, clinicians working in central Africa, for instance
Dr Bila Kapita, chief of internal medicine at
Hôpital Mama Yemo in
Kinshasa, reported that, at least since the mid-1970s, they started seeing cases that in retrospect were very likely to have been AIDS. This would be consistent with some degree of dissemination of the virus during the mid-1960s, given the average ten-year interval between infection and symptomatic disease. But could the disease have been present even earlier?
1
,
2
Bush medicinewhen
did the virus manage to cross species from chimps to humans? It has often been said that AIDS was a new disease on the African continent. Apart from the published cases mentioned in
Chapter 1
, clinicians working in central Africa, for instance
Dr Bila Kapita, chief of internal medicine at
Hôpital Mama Yemo in
Kinshasa, reported that, at least since the mid-1970s, they started seeing cases that in retrospect were very likely to have been AIDS. This would be consistent with some degree of dissemination of the virus during the mid-1960s, given the average ten-year interval between infection and symptomatic disease. But could the disease have been present even earlier?
1
,
2
In most district or regional hospitals of countries inhabited by
P.t. troglodytes
, the diagnostic facilities during the colonial era (and even now) were so minimal that it would have been difficult, even for astute and experienced clinicians, to recognise the emergence of a new disease characterised by intermittent fevers and profound wasting. Most such institutions did not have any kind of half-decent microbiology laboratory. No cultures were done, either for common bacterial pathogens or the agent of
tuberculosis, and diagnoses were based on stains made directly on the specimens, or solely on the combination of symptoms and signs found during the clinical examination. Fifty years later, I found the same situation at the
Nioki hospital in Zaire: nothing had changed. This approach was relatively effective for diagnosing parasitic diseases (malaria, sleeping sickness, filariasis, intestinal parasites) but very insensitive for most bacterial diseases. Little radiological investigation was available either; only in the best hospitals was it possible to get something as elementary as a chest x-ray. The first x-ray machine in Brazzaville was installed in 1931, two years before one became available in
Léopoldville.
P.t. troglodytes
, the diagnostic facilities during the colonial era (and even now) were so minimal that it would have been difficult, even for astute and experienced clinicians, to recognise the emergence of a new disease characterised by intermittent fevers and profound wasting. Most such institutions did not have any kind of half-decent microbiology laboratory. No cultures were done, either for common bacterial pathogens or the agent of
tuberculosis, and diagnoses were based on stains made directly on the specimens, or solely on the combination of symptoms and signs found during the clinical examination. Fifty years later, I found the same situation at the
Nioki hospital in Zaire: nothing had changed. This approach was relatively effective for diagnosing parasitic diseases (malaria, sleeping sickness, filariasis, intestinal parasites) but very insensitive for most bacterial diseases. Little radiological investigation was available either; only in the best hospitals was it possible to get something as elementary as a chest x-ray. The first x-ray machine in Brazzaville was installed in 1931, two years before one became available in
Léopoldville.
Thus a patient with fever, chronic diarrhoea and wasting might initially have been administered an antibiotic active against, say, typhoid fever. An old antibiotic, chloramphenicol, used to be popular for this indication. If this did not work, then extra-pulmonary tuberculosis would be suspected and the patient started on antituberculosis drugs (only after 1950 because, prior to that, there was no drug treatment for tuberculosis). Several weeks would be required to determine whether the patient improved on this second empirical medication. Some responded, and probably indeed suffered from occult tuberculosis
. Others did not and would slowly die, often at home after it had become clear that the hospital could not provide a solution, and the families did not want to waste all their meagre resources on unsuccessful therapeutic trials.
The doctors would presume that these patients died from some form of cancer, the diagnosis of which was well beyond the scope of bush hospitals. A final diagnosis would never be made, as doctors had too many other things to worry about to try to determine the actual cause of a particular death by performing an autopsy. The capacity to recognise an emerging disease was minimal, for the simple reason that there was a long list of serious diseases, already recognised in every medical textbook of the time, that these hospitals could not diagnose.
. Others did not and would slowly die, often at home after it had become clear that the hospital could not provide a solution, and the families did not want to waste all their meagre resources on unsuccessful therapeutic trials.
The doctors would presume that these patients died from some form of cancer, the diagnosis of which was well beyond the scope of bush hospitals. A final diagnosis would never be made, as doctors had too many other things to worry about to try to determine the actual cause of a particular death by performing an autopsy. The capacity to recognise an emerging disease was minimal, for the simple reason that there was a long list of serious diseases, already recognised in every medical textbook of the time, that these hospitals could not diagnose.
In the capitals, diagnostic facilities were better but still far from the European standards of the time, even in the clinics whose main (or only) role was to provide care for Europeans. These hospitals had a few specialists, mostly surgeons who could carry out biopsies if some form of cancer was suspected.
The histopathological slides would be sent to a collaborating hospital in Europe, and the results would come back months later. One such surgeon who worked in Brazzaville thought he had perhaps recognised a new disease, as we will see now.
The histopathological slides would be sent to a collaborating hospital in Europe, and the results would come back months later. One such surgeon who worked in Brazzaville thought he had perhaps recognised a new disease, as we will see now.
Léon Pales was not an ordinary colonial doctor. He graduated from Bordeaux in 1929, aged twenty-four. During his medical studies, to earn some money Pales worked as an anatomical assistant at the medical school, helping with autopsies and the dissection of cadavers for medical students learning anatomy, an experience that would later prove very useful
. While the usual MD thesis at the time consisted of a 60–80 pages literature review of some narrow medical topic, his was
429 pages long and addressed a very unusual field, palaeopathology: the study of diseases of prehistoric humans through examination of their bones. It would remain the standard French-language textbook for three decades. One of its main themes was that the study of ancient diseases could provide knowledge useful in understanding modern health problems. After the tropical medicine course in Marseilles, Pales was posted to
Moyen-Congo (1931–3) and
Tchad (1934–7). Back in France, he worked in
Marseilles, taught anatomy and ethno-anthropology at the
École du Pharo, and directed a field surgical unit during the invasion of France in 1940. Made a prisoner, he was repatriated to France the following year. He became assistant director of the
Musée de l’Homme in Paris but does not seem to have been involved in the resistance movement organised around this institution. After WWII, the rest of his career (in France, and a few years in West Africa) would be devoted to palaeopathology, his first love, to anthropology and nutrition
.
3
,
4
. While the usual MD thesis at the time consisted of a 60–80 pages literature review of some narrow medical topic, his was
429 pages long and addressed a very unusual field, palaeopathology: the study of diseases of prehistoric humans through examination of their bones. It would remain the standard French-language textbook for three decades. One of its main themes was that the study of ancient diseases could provide knowledge useful in understanding modern health problems. After the tropical medicine course in Marseilles, Pales was posted to
Moyen-Congo (1931–3) and
Tchad (1934–7). Back in France, he worked in
Marseilles, taught anatomy and ethno-anthropology at the
École du Pharo, and directed a field surgical unit during the invasion of France in 1940. Made a prisoner, he was repatriated to France the following year. He became assistant director of the
Musée de l’Homme in Paris but does not seem to have been involved in the resistance movement organised around this institution. After WWII, the rest of his career (in France, and a few years in West Africa) would be devoted to palaeopathology, his first love, to anthropology and nutrition
.
3
,
4
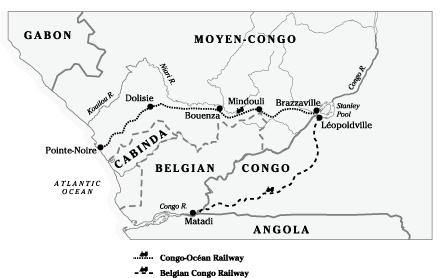
During his two-year term in Brazzaville, Pales’ career intersected with a colonial tragedy for the sake of ‘economic development’: the building of a railway between
Brazzaville and
Pointe-Noire, the Chemin de Fer Congo–Océan (CFCO), whose main purpose was to avoid depending on the Belgian railway. In a region with little infrastructure, a second railway was built only 100 kilometres from the
Matadi–Léopoldville line, at the same time as the latter was expanded (
Map 4
). Started in 1921, the 511-kilometre railway would not be completed until 1934. Ninety-two bridges or viaducts had to be erected, as well as twelve tunnels, with the longest stretching over 1.5 km. During construction, the regions immediately west of Brazzaville and east of Pointe-Noire presented no major logistical problem
; food could easily be delivered and the sick evacuated. In the middle, however, the 100-kilometre stretch
in the Mayombe, a dense and hilly equatorial rain forest, became a nightmare. The Mayombe was thinly populated and the workforce had to be imported, creating a huge melting pot of all
AEF ethnic groups, forced to live in squalid conditions highly propitious for the spread of microbial agents, perhaps including HIV-1.
5
Brazzaville and
Pointe-Noire, the Chemin de Fer Congo–Océan (CFCO), whose main purpose was to avoid depending on the Belgian railway. In a region with little infrastructure, a second railway was built only 100 kilometres from the
Matadi–Léopoldville line, at the same time as the latter was expanded (
Map 4
). Started in 1921, the 511-kilometre railway would not be completed until 1934. Ninety-two bridges or viaducts had to be erected, as well as twelve tunnels, with the longest stretching over 1.5 km. During construction, the regions immediately west of Brazzaville and east of Pointe-Noire presented no major logistical problem
; food could easily be delivered and the sick evacuated. In the middle, however, the 100-kilometre stretch
in the Mayombe, a dense and hilly equatorial rain forest, became a nightmare. The Mayombe was thinly populated and the workforce had to be imported, creating a huge melting pot of all
AEF ethnic groups, forced to live in squalid conditions highly propitious for the spread of microbial agents, perhaps including HIV-1.
5
Map 4
Itinerary of the Brazzaville–Pointe-Noire and Léopoldville–Matadi railways.
Itinerary of the Brazzaville–Pointe-Noire and Léopoldville–Matadi railways.
Initially in
Moyen-Congo, and later in
Oubangui-Chari and Tchad, 127,250 adult men were conscripted to work on the CFCO. Paid 1.5 francs per day, less than 1% of what their French foreman received, they worked ten hours a day, six days a week. Daily rations of food were inadequate, and the workers often received less than they were
supposed to. They were housed in mud-brick buildings, where 50–60 men slept in the same room. As rumours spread concerning the fate of CFCO workers, it became increasingly difficult for the local chiefs to recruit their target numbers, for many fled to safer areas. The colonial authorities lowered the age limit, increased the duration of forced labour and coerced some unfortunate men in returning up to five times. Some workers absconded, usually in groups, but escape was harder to envision for men from Oubangui-Chari and Tchad
. How could they possibly get back to their villages, a thousand kilometres away, without a penny in their pockets or any understanding of the local languages?
6
,
7
Moyen-Congo, and later in
Oubangui-Chari and Tchad, 127,250 adult men were conscripted to work on the CFCO. Paid 1.5 francs per day, less than 1% of what their French foreman received, they worked ten hours a day, six days a week. Daily rations of food were inadequate, and the workers often received less than they were
supposed to. They were housed in mud-brick buildings, where 50–60 men slept in the same room. As rumours spread concerning the fate of CFCO workers, it became increasingly difficult for the local chiefs to recruit their target numbers, for many fled to safer areas. The colonial authorities lowered the age limit, increased the duration of forced labour and coerced some unfortunate men in returning up to five times. Some workers absconded, usually in groups, but escape was harder to envision for men from Oubangui-Chari and Tchad
. How could they possibly get back to their villages, a thousand kilometres away, without a penny in their pockets or any understanding of the local languages?
6
,
7
Slave owners had an obvious interest in keeping their slaves alive: it was expensive to replace those who died. The situation was different with the CFCO. By contract, the AEF government had to supply the Société de Construction des
Batignolles with 8,000 workers year round. Their recruitment, transportation, lodging and feeding was the responsibility of the state. As soon as a worker died, the state had to provide another and pay a penalty to the company if the minimum number of workers was not available. This was an early example of a public–private partnership in which the private company got excellent terms.
Batignolles with 8,000 workers year round. Their recruitment, transportation, lodging and feeding was the responsibility of the state. As soon as a worker died, the state had to provide another and pay a penalty to the company if the minimum number of workers was not available. This was an early example of a public–private partnership in which the private company got excellent terms.
Grossly underpaid, underfed, overworked and housed in appalling conditions, between 15,000 and 23,000 workers died in the process, ten
times the death toll of the Léopoldville–
Matadi railway thirty years earlier. The most murderous section, and the most difficult from the engineers’ point of view, was the Mayombe. On top of the work accidents, epidemics broke out in the workers’ camps. Mortality among the Mayombe workers was a staggering 496 per 1,000 men-years in 1926 (in other words, half would be dead within a year), 454 in 1927 and 384 in 1928. It declined to 173 per 1,000 men-years in 1929, when sanitary conditions improved after this scandal was revealed in
France by writer André
Gide and journalist
Albert Londres. In absolute terms, the peak mortality occurred in 1927, when 2,892 workers died: eight per day. Mortality was highest among those recruited in Tchad
.
6
–
9
times the death toll of the Léopoldville–
Matadi railway thirty years earlier. The most murderous section, and the most difficult from the engineers’ point of view, was the Mayombe. On top of the work accidents, epidemics broke out in the workers’ camps. Mortality among the Mayombe workers was a staggering 496 per 1,000 men-years in 1926 (in other words, half would be dead within a year), 454 in 1927 and 384 in 1928. It declined to 173 per 1,000 men-years in 1929, when sanitary conditions improved after this scandal was revealed in
France by writer André
Gide and journalist
Albert Londres. In absolute terms, the peak mortality occurred in 1927, when 2,892 workers died: eight per day. Mortality was highest among those recruited in Tchad
.
6
–
9
Inspection missions were sent by the French government to investigate whether the newspaper reports were true, and to come up with solutions. Two military doctors,
General Lasnet and
Lieutenant-Colonel Ferris, led these inspections. Ferris described the pathetic conditions of the primitive hospitals set up near the building sites, where huts erected for twelve patients could house thirty, causing transmission of pathogens between patients.
Someone admitted for pneumonia ended up with
dysentery a few days later, or vice versa. The main causes of mortality were: dysentery (bloody diarrhoea), caused by
Shigella dysenteriae
, endemic in the Mayombe; pneumonia, caused by a bacterium known as the
pneumococcus;
beriberi, a vitamin B1 deficiency which causes heart failure; other ill-defined febrile illnesses; and what the doctors called ‘
physiological misery’, with some features (apathy, nostalgia) suggestive of major depression
.
6
,
10
General Lasnet and
Lieutenant-Colonel Ferris, led these inspections. Ferris described the pathetic conditions of the primitive hospitals set up near the building sites, where huts erected for twelve patients could house thirty, causing transmission of pathogens between patients.
Someone admitted for pneumonia ended up with
dysentery a few days later, or vice versa. The main causes of mortality were: dysentery (bloody diarrhoea), caused by
Shigella dysenteriae
, endemic in the Mayombe; pneumonia, caused by a bacterium known as the
pneumococcus;
beriberi, a vitamin B1 deficiency which causes heart failure; other ill-defined febrile illnesses; and what the doctors called ‘
physiological misery’, with some features (apathy, nostalgia) suggestive of major depression
.
6
,
10
The scandal in France and the inspection visits forced the AEF government to improve the workers’ sanitary conditions.
Governor Raphael Antonetti knew that he was in trouble and spent months writing detailed replies to the inspectors’ reports. Instructions about how to take proper care of the workers were issued. Wages were increased, and some women were allowed into the workers’ camps. Naturally,
prostitution quickly developed, and
STDs, hitherto inexistent, appeared among the workers. Prostitutes were noted to collect ‘their fees on paydays amidst long palavers’.
9
Governor Raphael Antonetti knew that he was in trouble and spent months writing detailed replies to the inspectors’ reports. Instructions about how to take proper care of the workers were issued. Wages were increased, and some women were allowed into the workers’ camps. Naturally,
prostitution quickly developed, and
STDs, hitherto inexistent, appeared among the workers. Prostitutes were noted to collect ‘their fees on paydays amidst long palavers’.
9
When Léon Pales arrived in Brazzaville in 1931 as the colony’s surgeon and obstetrician, the CFCO workers’ health situation had already
improved. Surgical facilities in Brazzaville were limited, so Pales had a lot of free time to do what he had learned in Bordeaux and which nobody in AEF had done before: autopsies.
He had access to the Institut
Pasteur laboratory, where bacteriological cultures were available (for instance, to look for pathogens causing diarrhoea, such as
Shigella
and
Salmonella
) and where guinea pigs could be inoculated to look for the aetiological agent of tuberculosis. The Pasteur laboratory was even able to characterise
pneumococci (the main agent of pneumonia) into serotypes.
improved. Surgical facilities in Brazzaville were limited, so Pales had a lot of free time to do what he had learned in Bordeaux and which nobody in AEF had done before: autopsies.
He had access to the Institut
Pasteur laboratory, where bacteriological cultures were available (for instance, to look for pathogens causing diarrhoea, such as
Shigella
and
Salmonella
) and where guinea pigs could be inoculated to look for the aetiological agent of tuberculosis. The Pasteur laboratory was even able to characterise
pneumococci (the main agent of pneumonia) into serotypes.
Pales eventually published a few scientific papers on this necropsic work. First, he reported the findings from eighty-five patients who had died from pneumococcal infections, sixty-four of whom were CFCO workers. The pneumococcus was grown from the blood cultures, the cerebrospinal fluid, pleural fluid, pericardial fluid or other specimens obtained either pre-mortem or during autopsy. Pales described the autopsy findings, from the adrenals to the brain, which often revealed disseminated pneumococcal infections. This did not imply that the patients were immunologically impaired, but reflected the absence of an effective treatment which allowed this virulent pathogen to spread throughout the body. It certainly demonstrated Pales’ unique competence and motivation in performing detailed autopsies and his access to the only laboratory in AEF where bacteriological cultures could be performed
.
11
–
12
.
11
–
12
He subsequently published a paper on tuberculosis in AEF, and more detailed information is available from a thesis written by medical student
Jean Auclert in
Marseilles using material provided by Pales. Pales described a new condition that he called Cachexie du Mayombe. Cachexia means profound weight loss. Adult male patients with Cachexie du Mayombe weighed as little as 30–5 kg, and were described as ‘an assembly of bones held together by skin . . . whose only sign of life lay in their gaze’. They had a normal appetite and experienced no vomiting but suffered from chronic non-bloody diarrhoea. However, repeated examination of their stools failed to reveal a parasitic agent, and stool cultures performed at the
Institut Pasteur were negative for the enteric pathogens known at the time, especially the
Shigella dysenteriae
which had killed many of the CFCO workers.
13
–
14
Jean Auclert in
Marseilles using material provided by Pales. Pales described a new condition that he called Cachexie du Mayombe. Cachexia means profound weight loss. Adult male patients with Cachexie du Mayombe weighed as little as 30–5 kg, and were described as ‘an assembly of bones held together by skin . . . whose only sign of life lay in their gaze’. They had a normal appetite and experienced no vomiting but suffered from chronic non-bloody diarrhoea. However, repeated examination of their stools failed to reveal a parasitic agent, and stool cultures performed at the
Institut Pasteur were negative for the enteric pathogens known at the time, especially the
Shigella dysenteriae
which had killed many of the CFCO workers.
13
–
14
Pales autopsied fifty such patients who, by his definition of the syndrome, had worked on the Mayombe part of the railway and sought care in Brazzaville after being declared unfit for service due to poor
health. In thirteen autopsies, he found confirmation of a tuberculosis that had been diagnosed pre-mortem, in seven others he found occult tuberculosis undiagnosed pre-mortem (tuberculosis of the intestine or the intra-abdominal lymph nodes), in four he found other diseases which killed the patient, but in twenty-six autopsies he did not find any macroscopically obvious medical condition explaining the profound wasting
. He did note, however, that many of these patients had cerebral atrophy, very unusual for young adults, and that they also had generalised lymphadenopathy, including large mesenteric (around the small bowel) lymph nodes, which failed to reveal the tuberculosis bacillus via staining and/or guinea pig inoculation. We do not know the actual incidence of the Cachexie du Mayombe, but Pales presumably autopsied only a small fraction of cases, as many must have died elsewhere than at the Brazzaville hospital.
health. In thirteen autopsies, he found confirmation of a tuberculosis that had been diagnosed pre-mortem, in seven others he found occult tuberculosis undiagnosed pre-mortem (tuberculosis of the intestine or the intra-abdominal lymph nodes), in four he found other diseases which killed the patient, but in twenty-six autopsies he did not find any macroscopically obvious medical condition explaining the profound wasting
. He did note, however, that many of these patients had cerebral atrophy, very unusual for young adults, and that they also had generalised lymphadenopathy, including large mesenteric (around the small bowel) lymph nodes, which failed to reveal the tuberculosis bacillus via staining and/or guinea pig inoculation. We do not know the actual incidence of the Cachexie du Mayombe, but Pales presumably autopsied only a small fraction of cases, as many must have died elsewhere than at the Brazzaville hospital.
This new syndrome was certainly suggestive of AIDS. We can be pretty sure that these twenty-six patients did not have disseminated tuberculosis or cancer, which should have been easy to recognise during the autopsy. Severe malnutrition was also unlikely, because the patients’ condition should have improved when properly fed in Brazzaville. The concentration of cases among patients who had worked in a well-defined area suggests a transmissible agent. Brain atrophy is common in patients with AIDS, and leads to a complication called AIDS dementia. Generalised lymphadenopathy is a hallmark of HIV infection, caused either by the virus itself or a variety of opportunistic infections which supervene. Such findings, as well as their chronic diarrhoea, would not have been noted had the patients died of major depression or some other severe psychological disturbance related to the hardship they had to endure.
One could speculate that the extremely high male/female ratio in the Mayombe work camps (ten men for each woman) and the intense
prostitution that ensued would have facilitated the transmission of HIV-1, possibly from a single worker who had been infected with SIV
cpz
. The time between the workers being sent to the CFCO camps and the development of their disease was not indicated in
Auclert’s thesis, but was probably less than the ten years we usually see today between getting HIV-1 and the first symptoms of AIDS. This does not exclude anything: for complex virological reasons, it is possible that this incubation period was actually shorter soon after the virus was introduced into human populations. And even nowadays, some unfortunate patients develop AIDS within two years after their infection
.
9
prostitution that ensued would have facilitated the transmission of HIV-1, possibly from a single worker who had been infected with SIV
cpz
. The time between the workers being sent to the CFCO camps and the development of their disease was not indicated in
Auclert’s thesis, but was probably less than the ten years we usually see today between getting HIV-1 and the first symptoms of AIDS. This does not exclude anything: for complex virological reasons, it is possible that this incubation period was actually shorter soon after the virus was introduced into human populations. And even nowadays, some unfortunate patients develop AIDS within two years after their infection
.
9
Unless the original tissue blocks or some of the slides prepared from the biopsies performed during these autopsies could be miraculously located, this will remain a hypothesis. I contacted the Pales family, the Institut Pasteur, the
Musée de l’Homme and Le Pharo, and no such material seems to have survived over the past seven decades. Unfortunately, there is no longer an Institut Pasteur in Brazzaville, and whatever archives may have existed seem to have been destroyed during the long periods of civil strife this country went through. So we will never know for sure. But the point that can be made from this story is that the supposed absence of a clinical condition recognised by early twentieth-century doctors cannot be used as a strong argument for dating the emergence of HIV
.
Musée de l’Homme and Le Pharo, and no such material seems to have survived over the past seven decades. Unfortunately, there is no longer an Institut Pasteur in Brazzaville, and whatever archives may have existed seem to have been destroyed during the long periods of civil strife this country went through. So we will never know for sure. But the point that can be made from this story is that the supposed absence of a clinical condition recognised by early twentieth-century doctors cannot be used as a strong argument for dating the emergence of HIV
.
Other books
The Table Talk of Samuel Marchbanks by Robertson Davies
The Race by Nina Allan
Son of Corse (The Raven Chronicles Book 2) by KateMarie Collins
Water For Elephants by Sara Gruen
Regarding the Events of One Sherlock’s Scandalous St. Valentine’s Day by Christine Danse
The Pull of Destiny by Hotcheri
Fortunes of War by Stephen Coonts
Lindsay's Surprise Crush by Angela Darling
Paper Covers Rock by Jenny Hubbard
The Adventures of Button by Richard W. Leech