Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine (72 page)
Read Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine Online
Authors: Marc Sabatine
Tags: #Medical, #Internal Medicine

BOOK: Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine
11.64Mb size Format: txt, pdf, ePub
•
Blastic phase
: TKI + HSCT vs. ALL or AML induction (based on cell type) + HSCT
•
Allogeneic HSCT
: consider for Pts w/ available donor who present in accelerated or blastic phase; reasonable option for Pts with relapsed/refractory disease to TKIs
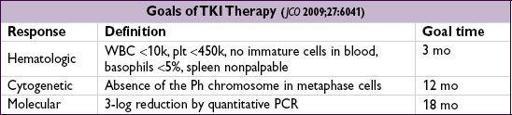
Prognosis
• Chronic phase CML Rx’d w/ imatinib: 89% overall survival, 95% survival free of CML-related deaths, 7% progression to blast phase at 5 y (
NEJM
2006;355:2408) • Accelerated phase CML Rx’d w/ imatinib: ~50% overall survival at 4 y (
Cancer
2005;103:2099) • Poor prognostic factors: ↑ age, ↑ platelet count, ↑ spleen size, ↑ percentage of blasts
CHRONIC LYMPHOCYTIC LEUKEMIA (CLL)
Definition
(
NEJM
2005;352:804;
Blood
2008;111:5446)
• Monoclonal accumulation of functionally incompetent mature B lymphocytes • CLL (>5000/µL malignant cells) & small lymphocytic lymphoma (SLL; <5000/µL malignant cells, but + LAN ± splenomegaly) now classified as same disease • Monoclonal B lymphocytosis (<5000/µL, nodes <1.5 cm, nl RBC and Plt counts): observe
Epidemiology and risk factors
• ~16,000 new cases/y; median age at dx is 72 y; most common adult leukemia • ↑ incidence in 1st-degree relatives; no known association with radiation, chemicals, drugs
Clinical manifestations
• Symptoms:
often asx
& identified when CBC reveals lymphocytosis; 10–20% p/w fatigue, malaise, night sweats, weight loss (ie, lymphoma “B” sx) • Signs:
lymphadenopathy
(80%) and
hepatosplenomegaly
(50%) •
Autoimmune hemolytic anemia
(AIHA) (~7%) or
thrombocytopenia
(ITP) (~1–2%) • Hypogammaglobulinemia ± neutropenia → ↑ susceptibility to
infections
• Bone marrow failure in
13%; monoclonal gammopathy in
5%
• Aggressive transformation: ~5% develop
Richter’s syndrome
= transformation into high-grade lymphoma (usually DLBCL) and sudden clinical deterioration
Diagnostic evaluation
(see “Lymphoma” for general approach)
•
Peripheral smear
:
lymphocytosis
(>5000/µL, mature-appearing small cells) “
smudge
” cells from damage to abnl lymphs from shear stress of making blood smear •
Flow cytometry
:
clonality
with dim surface Ig (sIg); CD5+, CD19+, CD20(dim), CD23+. CD38+ or ZAP70+ a/w unmutated Ig variable heavy chain region & worse prognosis.
•
Bone marrow
: normo-or hypercellular; infiltrated w/ small B-cell lymphocytes (≥30%) •
Lymph nodes
: infiltrated w/ small lymphocytic or diffuse small cleaved cells = SLL
•
Genetics
: del 11q22-23 & 17p13 unfavorable; trisomy 12 neutral; del 13q14 and mut
IgVH
favorable. Nine significantly mutated genes, including
TP53
,
NOTCH1
,
MYD88
and
SF3B1
. Key role for spliceosome mutations (
NEJM
2011;365:2497;
JCI
2012;122:3432).
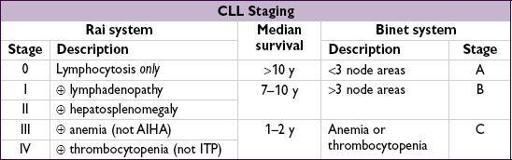
Treatment
• Treatment is primarily
palliative
→ early stage disease can be followed w/o Rx • Indications for treatment: Rai stages III/IV, Binet stage C, disease-related sx, progressive disease, AIHA or ITP refractory to steroids, recurrent infections • Options:
purine analogues
: fludarabine (“F”), pentostatin (“P”)
alkylating agents
: cyclophosphamide (“C”), bendamustine (“B”), CVP, CHOP; ? chlorambucil for elderly (lower response vs. F, butsurvival;
NEJM
2000;343:1750)
±
monoclonal Ab
against CD20 (
rituximab
, “R”) or CD52 (alemtuzumab, esp. w/ 17p-)
combination regimens
(eg, FR, FCR, BR) superior to monoRx (
Lancet
2007;370:230)
• Novel Rx refractory dis.: ofatumumab (ɑ-CD20), ibrutinib (BTK inhib), CAL101 (PI3K inhib) • Consider allo-HSCT in
p53
mut or refractory CLL (
BBMT
2009;15:53;
BJH
2012;158:174) • Supportive care: PCP, HSV, VZV prophylaxis; CMV monitoring for Pts receiving anti-CD52; AIHA/ITP → steroids; recurrent infections → IVIg
Prognosis
(
NEJM
2004;351:893;
JCO
2006;24:4634 & 2010;28:4473;
Blood
2008;111:865)
• Survival varies substantially. Median overall survival ~10 y (
Am J Hematol
2011;12:985) • Favorable prognosis: 13q14 deletion (~50% of CLL cases) • Factors a/w worse prognosis include:
unfavorable cytogenetics (eg, 17p-/
TP
53 mutation)
unmutated (<2% c/w germline)
IgVH
gene (<8–10 y vs. >20–25 y if mutated)
high (>20–30%) Zap-70 expression (part of T cell receptor; correlated w/ unmutated
IgVH
)
CD38 >30% or CD49d <30% (correlated with unmutated
IgVH
)
higher β
2
-microglobulin levels (correlate with disease stage and tumor burden)
LYMPHOMA
Definition
• Malignant disorder of lymphoid cells that reside predominantly in lymphoid tissues •
Hodgkin lymphoma
(HL) is distinguished from
non-Hodgkin lymphoma
(NHL) by
the presence of
Reed-Sternberg
(RS)
cells
Clinical manifestations
• Lymphadenopathy (nontender)
HL
: superficial (usually
cervical
/
supraclavicular
) ± mediastinal lymphadenopathy;
nodal
disease with
orderly
,
anatomic spread
to adjacent nodes
NHL
: diffuse;
nodal and extranodal
disease with
noncontiguous spread
; symptoms reflect involved sites (abdominal fullness, bone pain)
• Constitutional (“B”) symptoms:
fever
(>38°), drenching
sweats
, ↓
weight
(>10% in 6 mo)
HL
: periodic, recurrent “Pel-Ebstein” fever; 10–15% have pruritus; ~35% “B” symptoms
NHL
: “B” symptoms vary between types, ~15–50%
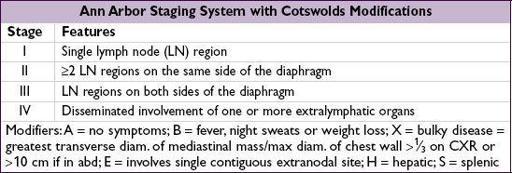
Diagnostic and staging evaluation
• Physical exam: lymph nodes, liver/spleen size, Waldeyer’s ring, testes (~1% of NHL), skin • Pathology:
excisional lymph node bx
(not FNA b/c need surrounding architecture) with immunophenotyping and cytogenetics;
BM
bx (except in HL clinical stage IA/IIA with favorable features or CLL clone by flow); LP if CNS involvement clinically suspected • Lab tests: CBC, BUN/Cr, LFTs, ESR, LDH, UA, Ca, alb; ✓ HBV & HCV (and must ✓ HBsAg & anti-HBc if planning rituximab Rx as can lead to HBV reactivation); consider HIV, HTLV, & EBV serologies and connective tissue diseases autoAbs • Imaging:
chest/abd/pelvic CT
, but doesn’t reliably detect spleen/liver involvement
consider
PET-CT scans
(esp. in HL, DLBCL). PET response to Rx can be prognostic (
Blood
2006;107:52;
JCO
2007;25:3746); has role to assess PR/CR after treatment.
Head CT/MRI
only
if neurologic symptoms.
HODGKIN LYMPHOMA (HL) (
NEJM
2010;363:653)
Epidemiology and risk factors
• ~9,000 cases/y; bimodal distribution (15–35 & >50 y); ↑; role of EBV in subsets of HL, esp. immunocompromised patients
Pathology
• Affected nodes show RS cells (<1%) in background of non-neoplastic inflammatory cells • Classic RS cells: bilobed nucleus & prominent nucleoli with surrounding clear space (“owl’s eyes”). RS cells are
clonal B-cells
: CD15+, CD30+, CD20– (rarely +).
Other books
Melody's Crush: (Book One) by Alora Dillon
So Shelly by Ty Roth
Those Jensen Boys! by William W. Johnstone
Hunger (Chicken Ranch Gentlemen's Club Book 1) by Amanda Young
Cold April by Phyllis A. Humphrey
Clifton County Fireworks by Joannie Kay
The Amen Cadence by J. J. Salkeld
The Landry News by Andrew Clements