Pediatric Examination and Board Review (204 page)
Read Pediatric Examination and Board Review Online
Authors: Robert Daum,Jason Canel

Boyd RL. Polyhydramnios and oligohydramnios. Emedicine Web site.
http://emedicine.medscape.com/article/975821-overview
. Accessed July 20, 2009.
Karrer FM. Duodenal atresia. Emedicine Web site.
http://emedicine.medscape.com/article/932917-overview
. Accessed July 20, 2009.
Minkes RK. Congenital anomalies of the esophagus. Emedicine Web site.
http://emedicine.medscape.com/article/934420-overview
. Accessed July 20, 2009.
CASE 114: NEONATE OF A DIABETIC MOTHER
You are caring for a full-term 4300-g infant girl who was delivered by cesarean delivery due to a failed attempt at a vaginal delivery after a long and difficult labor. Maternal membranes were ruptured for 26 hours, but there were no signs of chorioamnionitis at delivery. The mother had received six doses of IV ampicillin since admission. Despite the cesarean delivery, a vacuum extraction of the neonate from the uterus was noted in the delivery record. The mother was 34-years-old with a history of poorly controlled diabetes that was diagnosed when she was 15 years old. She has been noncompliant with her insulin regimen, and her HbA
1
C on admission was 10.6%. The mother fed her baby cow’s milk-based formula immediately after birth.
SELECT THE ONE BEST ANSWER
1.
What is the White classification of this mother?
(A) A2
(B) B
(C) C
(D) R
(E) F
2.
What is the next step in the evaluation of this infant?
(A) CBC
(B) serum electrolytes
(C) blood glucose
(D) infant serum insulin levels
(E) liver function panel
3.
As you examine this patient, you note tachypnea and nasal flaring. What is the most likely cause of this infant’s increased work of breathing?
(A) sepsis
(B) macrosomia
(C) pulmonary hypoplasia
(D) TTN
(E) congenital pneumonia
4.
The patient’s respiratory status has improved after spending 24 hours in a head hood with 100% oxygen, and on day of life 2, the infant is on room air and no longer tachypneic. She has not passed meconium by 36 hours of life. The baby has nonbilious vomiting and the abdomen is distended. The examination is also remarkable for a patent anus without stool in the rectal vault and a 4-cm raised, well-circumscribed, firm lump on the head where the vacuum was applied that does not cross the midline. The differential diagnosis includes all of the following except
(A) meconium plug
(B) Hirschsprung disease
(C) small left colon syndrome
(D) congenital hypothyroidism
(E) conjugated hyperbilirubinemia
5.
You order an abdominal x-ray that shows distended stool-filled loops of bowel with no signs of obstruction or free air. What is your next step in evaluating this patient?
(A) computed tomography of the abdomen
(B) upper GI with barium follow-through
(C) sweat test
(D) restart feedings slowly
(E) barium enema
6.
On day of life 4, you notice that the patient is jaundiced. There is no other abnormality in the physical examination. The indirect bilirubin level is 9 mg/dL and the total serum bilirubin is 10.3 mg/dL. The least likely cause of jaundice in this patient is
(A) breakdown of fetal red blood cell mass
(B) breakdown of extravascular blood
(C) Crigler-Najjar syndrome, type I
(D) immaturity of liver enzyme function
(E) delayed passage of meconium
7.
The mother tells you that the baby’s right arm, which you noted to be weak compared with the left arm on day of life 1, has not improved. When you examine the baby, you notice the right arm is limp and nonflexed. The Moro reflex is absent on the right side, but the grasp reflex is intact. All of the following are true about brachial plexus injuries except
(A) Erb palsy involves the upper trunk of the brachial plexus
(B) brachial plexus injury may cause respiratory distress
(C) lower brachial plexus injuries should prompt you to examine the pupils more closely
(D) most patients with brachial plexus injuries require surgical intervention
(E) Erb palsy is the most common brachial plexus injury
ANSWERS
1.
(C)
The White classification is used to ascertain risks to the fetus based on maternal age at onset of diabetes, duration of diabetes, and complications associated with diabetes. Class A
1
and class A
2
pertain to gestational diabetes (see
Table 114-1
).
2.
(C)
The most important initial evaluation in an infant born to a diabetic mother in the immediate postpartum period is to check the glucose level of the neonate. In utero, maternal glucose crosses the placenta, and, in response, the fetus; physiologic response is to create insulin. Once the neonate is delivered, the maternal glucose supply is interrupted but the fetal insulin effects are ongoing, causing neonatal hypoglycemia. Maternal insulin does not cross the placenta.
3.
(D)
This infant is at risk for TTN because she was born via cesarean delivery. It is postulated that infants born via cesarean delivery, not going through all the stages of labor, do not experience the catecholamine surge necessary to convert lung tissue ion channels from Cl
-
secretion to Na
+
reabsorption. This leads to retained fluid in the lungs. Although there was prolonged rupture of membranes, the mother received adequate intrapartum antibiotic prophylaxis, and there were no signs of chorioamnionitis at delivery, making sepsis and congenital pneumonia less likely. Macrosomia itself does not predispose an infant to TTN. There was no mention of congenital diaphragmatic hernia, so lung hypoplasia is not likely a concern.
4.
(E)
Failure to pass meconium after 48 hours warrants immediate attention. Of all the choices, only conjugated hyperbilirubinemia would not present with delayed passage of stool. Meconium plug syndrome is common in infants born to diabetic mothers. This disease process occurs typically in term infants and is usually self-limited. Depressed or hypotonic neonates, including those whose mothers were receiving magnesium sulfate, are also at risk for meconium plug syndrome. Meconium ileus is seen in neonates with cystic fibrosis. Hirschsprung disease and small left colon syndrome have identical presentations, and radiographic findings but can be differentiated on rectal biopsy. In Hirschsprung disease, the biopsy shows no ganglions in the submucous or myenteric plexuses. Some consider small left colon syndrome pathognomonic of infants born to diabetic mothers. In addition to delayed passage of meconium, infants with congenital hypothyroidism may be jaundiced, have a large umbilical hernia, coarsened facies, a large anterior fontanelle, and hypotonia.
TABLE 114-1
Modified White’s Classification of Diabetes in Pregnancy
| CLASS | DESCRIPTION |
| A | Abnormal glucose tolerance test (GTT) at any age or of any duration treated only by diet therapy |
| B | Onset at age 20 years or older and duration of less than 10 years |
| C | Onset at age 10-19 years or duration of 10-19 years |
| D | Onset before 10 years of age, duration over 20 years, benign retinopathy, or hypertension (not preeclampsia) |
| D1 | Onset before age 10 years |
| D2 | Duration over 20 years |
| D3 | Calcification of vessels of the leg (macrovascular disease), formerly called Class E |
| D4 | Benign retinopathy (microvascular disease) |
| D4 | Hypertension (not preeclampsia) |
| R | Proliferative retinopathy or vitreous hemorrhage |
| F | Nephropathy with more than 500 mg/day proteinuria |
| RF | Criteria for both classes R and F |
| G | Many pregnancy failures |
| H | Evidence of arteriosclerotic heart disease |
| T | Prior renal transplantation |
| Gestational Diabetics | |
| A1 | Diet-controlled gestational diabetes |
| A2 | Insulin-treated gestational diabetes |
Classes B through T require insulin treatment. Adapted from Hare JW, White JP. Gestational diabetes and the White classification. Diabetes Care. 1980;3:394.
5.
(E)
The next step in the evaluation of delayed passage of meconium would be a barium enema with rectal biopsy. Because Hirschsprung disease and small left colon are indistinguishable radiographically, a rectal biopsy is necessary to differentiate between the two. A barium enema is also therapeutic for small left colon syndrome.
6.
(C)
All the choices may cause indirect hyperbilirubinemia in an infant at this age, but the level of unconjugated bilirubin found in Crigler-Najjar syndrome, type I would be much higher for an affected infant at day of life 4. The 4-cm lump previously described is a cephalohematoma (blood in the subperiosteum), which also can contribute to indirect hyperbilirubinemia.
Jaundice is a frequent issue in newborns. To understand why an infant is jaundiced, it is important to know the life cycle of bilirubin; there are three sites in this pathway where problems with bilirubin overload can occur: reticuloendothelial system (RES), liver, and GI system (see
Figure 114-1
).
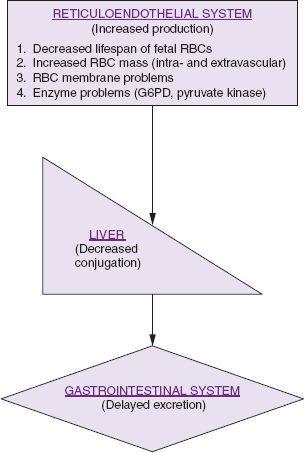
FIGURE 114-1.
Life cycle of bilirubin.
7.
(D)
Erb palsy involves the upper brachial plexus (C5-C7), and Klumpke palsy involves the lower brachial plexus (C8-T1). Erb palsy is more common. A patient with Erb palsy presents with the affected arm in a nonflexed position, assuming the classic waiter’s tip appearance; grasp is usually unaffected. An infant with Klumpke palsy holds the arm supinated, with the elbow bent and the wrist extended; the grasp is usually weak. More severe BPIs can lead to Horner syndrome (miosis in affected pupil) or diaphragmatic paralysis due to phrenic nerve injury. Most cases of BPI are selflimited and do not require surgical intervention. Risk factors for BPIs include large-for-gestationalage infants, shoulder dystocia, infants of diabetic mothers, and use of forceps or vacuum at delivery.