Pediatric Examination and Board Review (202 page)
Read Pediatric Examination and Board Review Online
Authors: Robert Daum,Jason Canel

FIGURE 112-3A.
Reticulogranular pattern with air bronchograms.
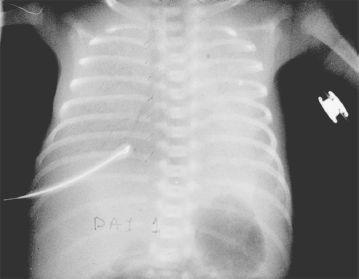
FIGURE 112-3B.
Chest radiograph showing “whiteout” in severe respiratory distress syndrome.
5.
(E)
A normal ABG determination for a premature baby on day 1 of life would be pH higher than 7.25, Paco
2
of 45-55 mm Hg, and a Pao
2
>50 mm Hg. The normal cord blood glucose is 80% of the mother’s glucose but reaches a nadir at about 2 hours of age but is less than 45 mg/dL. A general rule of thumb is that the mean BP is roughly the same as the gestational age. For this baby, a mean BP higher than 26 mm Hg is normal. Insensible water loss is inversely proportional to gestational age; that is, the more immature the baby, the higher the insensible water loss. Because premature babies lighter than 750 g have very high insensible water losses, the serum Na should be monitored closely and the fluid administration adjusted accordingly. The serum Ca of a neonate on day 1 of life is normally higher than that of the mother. Therefore, the patient does not need any Ca added to the IV fluids on day 1 of life. Babies lighter than 750 or 1000 g are sometimes placed on prophylactic phototherapy on day 1 of life. An O
2
saturation in the high 80% to the low 90% range is acceptable on day 1 of life. NICUs have different standards for an acceptable O
2
saturation at different times of a premature baby’s life, and thus these values may very slightly.
6.
(A)
A serum Na of 150 mEq/mL indicates that the insensible water loss was underestimated. One should increase the volume of administered fluids and continue to monitor serum electrolytes. The baby’s weight also should be monitored. It is necessary to monitor the serum glucose because the fluid volume being administered is increased. If the serum glucose is normal, D10W can be given. If the serum glucose is high, a change to D5W should be made as you increase the administered fluid volume. The baby should lose weight in the first few days. A weight loss of 1-3% per day is called physiologic dehydration and is desirable.
7.
(E)
The serum Na concentration is now 152 mEq/mL, so it would be appropriate to increase the total fluids being administered. Because the serum Ca is low, it would be appropriate to add Ca. Blood gases suggest overventilation, so it would be appropriate to adjust the ventilatory settings. Hyperalimentation is usually started in extremely low-birthweight babies on day 1-2 of life.
8.
(A)
Urine is the main avenue of K excretion. Once the urine output is good, K can be added to the IV fluids if the serum K is not high. Because the serum Na is still high, the rate of fluid administration should be increased. In premature babies lighter than 750 g that are not oliguric, hyperkalemia can occur. If a patient’s serum K is 7.5-8, one should not dismiss it as a laboratory error or secondary to hemolysis.
9.
(B)
The fetal ductus arteriosus (DA) is a normal structure in utero allowing blood to bypass the fetal pulmonary vascular bed and go directly to the descending aorta. The DA is kept patent by prostaglandin E2. Functional closure of the DA occurs at about 15 hours of life and is triggered by increasing Pao
2
. True anatomic closure of the DA, where reopening is not possible, may take several weeks. The clinical signs of PDA are widened pulse pressure, an active precordium, full or bounding pulses, and a pansystolic murmur. An echocardiogram and a chest radiograph should be obtained.
Excessive fluid administration has been associated with an increased incidence of PDA. Indomethacin, a prostaglandin inhibitor, is an effective treatment.
10.
(D)
Congenital infection with rubella has been classically associated with PDA. Myocarditis may be a feature of congenital syphilis, but usually one thinks of the typical rash associated with syphilis, snuffles, and bony abnormalities with regard to congenital syphilis. Congenital varicella syndrome is often associated with eye findings, microcephaly, fibrous scars, and limb hypoplasia. Congenital CMV infection often has periventricular intracranial calcifications, chorioretinitis, sensorineural hearing loss, and skin findings. Congenital parvovirus B19 may lead to hydrops fetalis in utero.
11.
(D)
Indomethacin is associated with vasoconstriction of other vessels including the cerebral, mesenteric, and renal vasculature. Renal function should be assessed before giving indomethacin. Urine output less than 1 mL/kg per hour or a serum creatinine more than 1.8 mg/dL is a contraindication to the use of indomethacin. Dilutional hyponatremia has also been reported.
12.
(E)
Abdominal distention and increased gastric residuals before feeding may be signs of NEC. The diagnosis of NEC is made by abdominal radiograph. Because infection plays a role in the pathogenesis of NEC, a sepsis workup should be done and the patient should be started on antibiotics.
13.
(E)
The abdominal radiograph is suggestive of pneumatosis intestinalis. There is no free air and no portal air. NEC is predominantly a disease of premature babies, although 10% of cases occur in term infants. Signs and symptoms of NEC vary and may include apnea and bradycardia, vomiting, increased residuals, abdominal distention, and heme-positive stools. The diagnostic hallmark of NEC is pneumatosis intestinalis or submucosal air on an abdominal radiograph. Once the radiographic diagnosis of NEC is made, serial abdominal radiographs should be done looking for free air. The platelet count should be monitored. A drastic drop in the platelet count is an ominous sign. Because patients can lose a large amount of fluid into the abdominal cavity (third spacing), urine output should be monitored closely. A patient with NEC may require large amounts of IV fluids. It is important to monitor ABGs. Intractable acidosis is an ominous sign. Recent studies have shown that early feeding with probiotics may decrease the incidence of NEC, but if NEC is already clinically suspected, the patient must be made NPO; there is no evidence that probiotics will help treat NEC.
14.
(A)
The patient in
Figure 112-2
has free air in the abdomen, an absolute indication for surgery. Other findings such as the fixed loop sign, intractable thrombocytopenia, intractable acidosis, and signs of peritonitis are relative indicators used by surgeons to decide about the need for laparotomy. All these relative indications point to the possibility of necrotic intestine in the abdomen.
15.
(A)
Strictures happen in about 10% of patients following NEC. Sepsis at this point is related to physician interventions such as indwelling vascular catheters placed for prolonged hyperalimentation.
16.
(A)
Periventricular or intraventricular hemorrhage can occur in 20-30% of premature babies; 90% of the hemorrhages occur in the first 72 hours of life. Fifty percent of the hemorrhages are clinically silent; others may present with subtle clinical change. A catastrophic presentation with a bulging anterior fontanel, drop in hematocrit, metabolic acidosis, and hyperglycemia can also occur. All premature babies lighter than 1500 g or less than 32-34 weeks’ gestation should have a first ultrasound of the head at day 3-5 of life, a second at day 7-10 of life, and subsequent ultrasounds based on these early results.
Intraventricular hemorrhages are classified as follows:
| Grade I | Subependymal bleed with no intraventricular extension |
| Grade II | Intraventricular hemorrhage with no ventricular dilation |
| Grade III | Intraventricular hemorrhage with ventricular dilation |
| Grade IV | Intraparenchymal bleed |
Retinopathy of prematurity (ROP) is a disorder of developing retinal blood vessels that continues to be a cause of major visual morbidity in premature infants. All premature infants should have an eye examination for ROP at about 4 weeks of age and continued periodic examinations until the retina is completely vascularized.
 S
S
UGGESTED
R
EADING
Henry MCW, Moss RL. Current issues in the management of necrotizing enterocolitis.
Semin Perinatol.
2004;28;221-233
CASE 113: A TERM NEONATE WITH A HISTORY OF MATERNAL POLYHYDRAMNIOS
A 37-week gestational age, 2800-g baby girl is born to a 20-year-old primigravida by normal, spontaneous vaginal delivery. The pregnancy is significant for polyhydramnios. The baby’s Apgar scores are 8 and 9 at 1 and 5 minutes, respectively. The baby looks good, is pink on room air, in no distress, and is sent to the regular nursery.
SELECT THE ONE BEST ANSWER
1.
Which of the following choices primarily controls the volume of amniotic fluid?
(A) fetal urine output
(B) family history
(C) placental factors
(D) gender of fetus
(E) fetal effluence from the gut
2.
Which of the following statements about amniotic fluid is true
?
(A) the swallowing ability of the fetus is a determinant of amniotic fluid volume
(B) at term the average volume of amniotic fluid is 3-5 L