Pediatric Examination and Board Review (172 page)
Read Pediatric Examination and Board Review Online
Authors: Robert Daum,Jason Canel

(D) nosocomial urinary tract infection caused by
Enterococcus faecalis
in a hospitalized 3-yearold child
(E) Group B streptococcal meningitis in a neonate
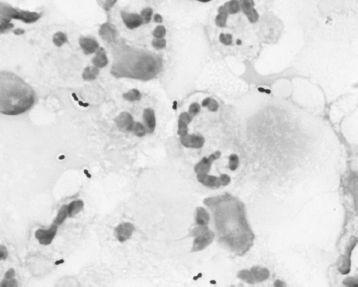
FIGURE 98-1.
Gram stain of CSF that grew
S pneumoniae
revealing gram-positive diplococci. Note halo surrounding some of the organisms that represents the capsule. See color plates.
3.
The penicillinase-resistant penicillin oxacillin is not inactivated by the action of the bacterial penicillinase. Oxacillin would therefore be effective therapy for treatment of which of the following infections?
(A)
Enterococcus faecalis
bacteremia
(B)
Pasteurella multocida
wound infection caused by a cat bite
(C) methicillin-susceptible
S aureus
cellulitis of the lower leg
(D) methicillin-resistant coagulase-negative staphylococci causing a ventriculoperitoneal shunt infection
(E)
E coli
urinary tract infection
4.
Ampicillin is appropriate therapy for which of the following infections?
(A) beta-Lactamase producing
Moraxella catarrhalis
(B) ESBL-producing
Klebsiella pneumoniae
(C) MSSA causing pneumonia in a 12-month-old child
(D)
Clostridium difficile
causing diarrhea in a 4-year-old hospitalized child
(E)
Listeria monocytogenes
causing meningitis in a 3-week-old infant
5.
A 3-year-old child recently diagnosed with acute myelogenous leukemia (AML) has received induction chemotherapy. The child is admitted to the children’s hospital because of fever, neutropenia, and hypotension. The best initial empirical antimicrobial therapy would include
(A) ceftazidime
(B) ceftriaxone and tobramycin
(C) clindamycin and ceftriaxone
(D) vancomycin
(E) ampicillin and gentamicin
6.
A 6-week-old infant presents to your office with the insidious onset of cough and tachypnea. On examination the infant is afebrile with rales on pulmonary auscultation. You suspect
Chlamydia trachomatis
pneumonia that is supported by a chest radiograph demonstrating interstitial infiltrates. Erythromycin is prescribed and you tell the infant’s mother that the most common adverse reaction of erythromycin is
(A) cholestatic jaundice
(B) gastrointestinal (GI) discomfort
(C) hearing loss
(D) maculopapular rash
(E) infantile hypertrophic pyloric stenosis
7.
Of the following situations, azithromycin would be most appropriate for treatment of which infection?
(A) a 5-year-old boy with group A streptococcal pharyngitis
(B) a 2-year-old with impetigo caused by MRSA
(C) a 4-year-old child with lobar pneumonia caused by
S pneumoniae
that is resistant (MIC = 2.0 μg/mL) to penicillin
(D) a 15-year-old adolescent girl with
C trachomatis
cervicitis
(E) a 6-year old girl with
Pseudomonas aeruginosa
urinary tract infection
8.
An 18-month-old boy develops anterior cervical lymphadenitis requiring drainage of an abscess that has formed. The abscess culture grows MRSA that is D-test negative. The most appropriate antibiotic for treatment would include
(A) vancomycin
(B) imipenem
(C) cefepime
(D) cefazolin
(E) clindamycin
9.
A 5-year-old boy whom you follow for short bowel syndrome has a central venous catheter infection. He is admitted to the children’s hospital with fever to 104°F (40°C). He is also known to be colonized with MRSA. A central line infection is strongly suspected and vancomycin is started. The blood culture grows vancomycin-resistant
E faecalis
. Appropriate therapy would now include
(A) linezolid
(B) meropenem
(C) clindamycin
(D) clofazimine
(E) ceftazidime
10.
A 13-year-old adolescent boy with HIV infection is being treated with trimethoprim-sulfamethoxazole (TMP-SMX) for
Pneumocystis jiroveci
pneumonia. Adverse reactions that can occur during TMP-SMX therapy include all but
(A) Stevens-Johnson syndrome
(B) neutropenia
(C) renal dysfunction
(D) pancreatitis
(E) diarrhea
11.
Sulfonamides such as sulfadiazine, sulfamethoxazole, and sulfisoxazole all have indications for clinical use in infants and children for all of the following except
(A) congenital toxoplasmosis
(B) prophylaxis of urinary tract infections
(C) ulcerative lesions caused by
Nocardia
(D) meningitis caused by
Neisseria meningitidis
(E) chlamydial conjunctivitis
12.
A 2
1
/
2
-year-old girl with a ventriculoperitoneal shunt placed after an intraventricular hemorrhage (IVH) occurring as a premature neonate develops fever to 102.2°F (39°C), vomiting, and irritability. Examination of the CSF reveals pleocytosis and a Gram stain showing a few gram-positive cocci in clusters. You start empirical therapy with vancomycin. All of the following are appropriate uses of vancomycin except
(A) treatment of serious infections attributable to beta-lactam-resistant gram-positive organisms
(B) treatment of infections attributable to grampositive microorganisms in patients with serious allergy to beta-lactam agents
(C) empiric antimicrobial therapy for a febrile neutropenic patient
(D) prophylaxis for major surgical procedures involving implantation of prosthetic materials or devices at institutions with a high rate of infection caused by MRSA
(E) treatment of
Clostridium difficile
colitis that fails to respond to metronidazole therapy
13.
A 5-year-old boy from New York comes to your office with a swollen, tender left knee and some limitation of motion. His mother remembers the child having been bitten by a tick a few months ago during the summer. You suspect Lyme disease, which is confirmed by serology. The mother was treated for Lyme disease 2 years ago with doxycycline and wonders if her child should also be treated with doxycycline. You tell her that
(A) doxycycline is only indicated for early Lyme disease with erythema migrans
(B) ceftriaxone is the antibiotic of choice for initial treatment of Lyme arthritis in children
(C) doxycycline can cause permanent dental discoloration in children younger than 8 years
(D) doxycycline is the antibiotic of choice if the arthritis does not initially respond to treatment with amoxicillin
(E) doxycycline is the recommended treatment if Lyme disease is complicated by meningitis
14.
A 4-year-old child with
Streptococcus viridans
group endocarditis is being treated with penicillin and gentamicin. The following statement best describes the nephrotoxicity caused by the use of aminoglycosides
(A) aminoglycosides vary markedly in their risk for nephrotoxicity
(B) nephrotoxicity can be increased by the concomitant use with cyclosporine
(C) the dose of aminoglycosides is not correlated with development of nephrotoxicity
(D) gentamicin nephrotoxicity is usually irreversible
(E) nephrotoxicity is not related to the duration of aminoglycoside exposure
15.
A 4-year-old girl returns from a trip to Pakistan with her family. She develops fever, headache, and abdominal pain that persists for 1 week. She has mild intermittent diarrhea and a rash develops in the second week of the illness.
Salmonella typhi
is isolated from blood that is ampicillin resistant but chloramphenicol susceptible. The most common adverse effect occurring with chloramphenicol use includes
(A) gray baby syndrome
(B) aplastic anemia
(C) ototoxicity
(D) myocardial toxicity
(E) dose-dependent anemia with low reticulocyte count
16.
The use of fluoroquinolones in the pediatric age group has been limited because fluoroquinolones cause cartilage damage in puppies and large joint arthropathy in other immature animals. Their use in children therefore has not been approved by the FDA except for ciprofloxacin, which has been approved for complicated urinary tract infections, pyelonephritis caused by
E coli,
and postexposure prophylaxis for inhalation anthrax. Nevertheless, there has been an increasing experience in children with the use of fluoroquinolones in certain situations. Which of the following scenarios is a clinical situation in which the use of a fluoroquinolone is inappropriate?
(A) pulmonary exacerbation in cystic fibrosis patient
(B) cellulitis caused by MRSA
(C) typhoid fever caused by
S typhi
resistant to ampicillin, ceftriaxone, and TMP-SMX
(D) urinary tract infection caused by
Pseudomonas aeruginosa
(E) part of an initial multidrug regimen for inhalational anthrax
17.
A 4-year-old girl has had daily contact with her aunt for the past 2 months. The aunt has recently been diagnosed with isoniazid-resistant pulmonary tuberculosis. A chest radiograph of the child is normal. Appropriate treatment of the child includes
(A) azithromycin
(B) ethambutol
(C) rifampin
(D) clofazimine
(E) linezolid
18.
A 6-year-old boy develops an intra-abdominal abscess following appendectomy for a ruptured appendix. Meropenem is being administered as part of empiric therapy. Organisms that are susceptible to meropenem include