Pediatric Examination and Board Review (169 page)
Read Pediatric Examination and Board Review Online
Authors: Robert Daum,Jason Canel

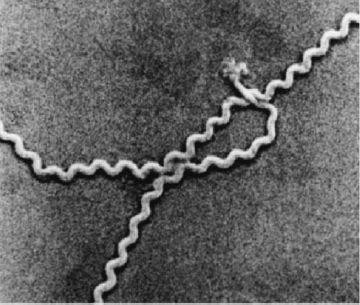
FIGURE 96-1.
Scanning electron micrograph of leptospires. (Reproduced, with permission, from Fauci AS, Kasper DL, Braunwald E, et al. Harrison’s Principles of Internal Medicine, 17th ed. New York: McGraw-Hill; 2008: Fig. 164-1.)
6.
(B)
Chemoprophylaxis is indicated for childcare contacts of a child with pertussis infection. Chemoprophylaxis in child-care settings is also recommended for meningococcal disease. Chemoprophylaxis is also recommended when 2 or more cases of invasive
H influenzae
type b disease have occurred within 60 days, although such an event is exceedingly rare in the vaccine era. No chemoprophylaxis, however, is recommended for people exposed to a patient with serotype f disease.
7.
(D)
All frequently touched toys in rooms where infants and toddlers stay should be cleaned and disinfected daily, but it is not necessary to remove them. For older children who are toilet trained, toys should be cleaned weekly and when soiled.
8.
(D)
Children with HIV infection do not need to be excluded from child care. Standard precautions should be adopted by the child-care center for handling spills of blood and blood-contaminated body fluids and wound drainage of all children. Transmission of HIV has not occurred through day-to-day contact in child-care centers. Child-care providers do not need to be informed of the HIV status of any child attending child care.
9.
(E)
In this scenario, there is only indirect contact; that is, the only contact is with a high-risk contact but no direct contact with the index patient. This is a low-risk situation, and chemoprophylaxis is not recommended (
Table 96-1
).
10.
(B)
Children with
Salmonella
gastroenteritis may return to day care once they are asymptomatic. Approximately 50% of children younger than 5 years continue to excrete
Salmonella
for 12 weeks after infection. Antimicrobial therapy is not indicated for uncomplicated
Salmonella
gastroenteritis because therapy does not shorten the disease course and may prolong duration of carriage.
11.
(C)
All symptomatic individuals in a child-care facility with
Shigella
infection should receive antimicrobial therapy. In mild disease, the primary indication for treatment is to prevent spread of
Shigella
throughout the day-care center. Child-care attendees or staff members with symptomatic infection should be excluded until the diarrhea has resolved.
12.
(E)
The correct transmission-based precautions in the hospital setting to prevent transmission of RSV infection is contact precautions.
TABLE 96-1
Chemoprophylaxis For Contacts of Individuals With Invasive Meningococcal Disease
| HIGH RISK (RECOMMENDED) | LOW RISK (NOT RECOMMENDED) | REGIMENS |
Household contact | Casual contact (no exposure to oral secretions) | Rifampin (2 days, bid both days) |
Childcare contact ≤7 days before illness | Indirect contact (only contact is high-risk contact) | Ceftriaxone (single dose) |
Direct exposure to index patient’s secretions (kissing, sharing toothbrush or utensils) | Health-care professional with no direct exposure to patient’s oral secretions | Ciprofloxacin (single dose) |
Mouth-to-mouth resuscitation, intubation, suctioning | ||
Frequently slept/ate in same dwelling during 7 days before onset of illness |
13.
(C)
In the hospital setting, the correct transmissionbased precautions to prevent spread of
Mycobacterium tuberculosis
is airborne precautions. Children younger than 12 years of age with pulmonary tuberculosis are rarely contagious because cavitary disease is rare and cough is not productive so there is little or no expulsion of bacilli, although precautions are generally instituted nevertheless. If a patient is receiving adequate antituberculosis therapy with cough resolved and 3 sputum smears (if available) are negative for acid-fast bacilli, the person can be considered noncontagious.
14.
(C)
Child-care or school providers need not be informed of the HIV status of a child who is attending a child-care center or school. In the absence of blood exposure, HIV is not acquired through the types of contact that occur in school settings, including contact with saliva or tears. HIV transmission among adolescents is attributed primarily to two categories of sexual contact: heterosexual or between MSM.
15.
(B)
There is no increased risk of transmission of hepatitis B infection in the school setting. An exception is that residents and staff of institutions for people with developmental disabilities represent a high-risk group for hepatitis B virus infection and should be immunized. In the clinical situation in the question, the classmate of the 12-year-old who is the hepatitis B surface antigen positive should complete the 3-dose series. It is not necessary to begin the series again even though the last dose of vaccine was 1 year previously.
16.
(E)
The risk of transmission from a percutaneous needle accident is highest with hollow-bore needles. Antiretroviral therapy is generally not recommended if the source of a needlestick injury is not known in the nonoccupational setting, such as injuries from discarded needles. Finally, needlestick injuries can also result in hepatitis C virus transmission.
17.
(D)
Household contacts are in the high-risk category for contacts of individuals with meningococcal disease. Rifampin, ceftriaxone, or ciprofloxacin can be used for chemoprophylaxis (
Table 96-1
).
18.
(D)
Children living in residential institutions should receive all the routine childhood vaccines. In this setting children as well as staff are at increased risk of acquiring hepatitis B virus infection. Outbreaks of hepatitis A virus infection can occur in residential institutions. The routine vaccination of all children 1 year of age and older is now recommended. Hepatitis A vaccine, in addition to immunoglobulin, should be considered for staff and residents in an institutional setting where an outbreak of hepatitis A is occurring. An unimmunized 2-year-old child who lacks a history of varicella or herpes zoster diagnosed by a health-care professional, should also receive varicella vaccine. MCV4 is only recommended for children in the age group 2-10 years with a high-risk condition.
 S
S
UGGESTED
R
EADING
Pickering LK, Baker CJ, Kimberlin DW, Long SS.
Red Book
:
2009 Report of the Committee on Infectious Diseases.
28th ed. Elk Grove Village, IL: American Academy of Pediatrics; 2009.
Robinson J. Infectious diseases in schools and childcare facilities.
Pediatr Rev.
2001;22:39-46.
CASE 97: A 3-YEAR-OLD WITH A FEBRILE SEIZURE
You are called during the middle of a busy day at the office on a Friday afternoon by the pediatric resident at the children’s hospital emergency department. You have been very busy all week, seeing many children of all ages with fever associated with upper respiratory tract symptoms (especially cough, rhinorrhea, and sore throat). The pediatric resident tells you that one of your patients, a 3-year-old previously healthy child, was brought to the emergency department after being witnessed by parents at home to have a 5- to 10-minute episode of shaking of the arms and legs. The shaking of the arms and legs had stopped while en route to the emergency department with the parents.
At the emergency department the child was noted to be sleepy and nonresponsive. The temperature was 103.1°F (39.5°C). There was minimal nasal congestion. The throat was erythematous. The neck was supple; bilateral anterior cervical adenopathy was present. The spleen tip was palpable. Examination of both lungs and the heart were normal.
SELECT THE ONE BEST ANSWER
1.
Because it is December and you have been seeing many children with febrile respiratory illnesses in your office, you suspect influenza is the etiology. The most rapid and sensitive method to diagnose influenza A infection is
(A) viral culture of nasopharyngeal specimen
(B) Influenza A EIA antigen detection on throat specimen
(C) Influenza A DFA on nasopharyngeal specimen
(D) Influenza A IgM serology on acute serum
(E) Influenza A (immunochromatographic rapid antigen) test on nasopharyngeal specimen
2.
The evaluation for influenza A in the child with the febrile seizure does not confirm that diagnosis. You next consider adenovirus in the differential diagnosis. The best method to diagnose adenovirus includes
(A) “shell vial” culture of nasopharyngeal specimen
(B) polymerase chain reaction (PCR) on nasopharyngeal specimen
(C) adenovirus DFA on nasopharyngeal specimen
(D) adenovirus complement fixation (IgG) antibody on convalescent serum
(E) adenovirus neutralizing (IgG) antibody on acute and convalescent serum