Obsessive Compulsive Disorder (8 page)
Read Obsessive Compulsive Disorder Online
Authors: Polly Waite

36
Gallop
Mild obsessions and rituals occur as normal developmental phenomena in children (Evans
et al.
, 1997) and differ from obsessive compulsive symptoms in several ways. Most normal rituals and fears do not usually cause distress or interfere with the child’s day-to-day functioning. Normal fears and rituals also occur at specific stages and are then outgrown whereas OCD rituals and worries persist and are developmentally inappropriate. Developmentally appropriate fears tend to be about normal day-to-day themes, whereas although obsessions can be about normal topics, they are often unrealistic or disproportionate to the actual threat. It is therefore helpful for the therapist not only to bear in mind these distinctions when assessing for the presence of both early and current obsessions and compulsions, but also to ask the young person if they feel this is a ‘normal worry/behaviour or an OCD one’ as most are able to make this distinction.
It is hypothesised that certain beliefs (e.g. about inflated responsibility, thought and action and cognitive control etc.) emerge from early childhood experience and that these beliefs may be associated with the development of OCD (Rachman and Hodgson, 1980; Salkovskis
et al.
, 1999). The therapist should therefore find out about any experiences where the child: • is given too much responsibility
• is exposed to rigid or extreme codes of conduct or duty
• is left feeling incompetent after being shielded from taking responsibility
• is left feeling actively or passively responsible for significant events or misfortune
• learned that they should be moral in all thought and actions
• learned that they should always have control over their thoughts
• learned that thinking something is equivalent to taking action.
Significant precipitating incidents such as discrete life events or ongoing stressful situations or transitions within the family, at school or involving the media should also be noted, given that a significant proportion of children with OCD develop symptoms following such incidents (Rettew
et al.
, 1992).
Once possible vulnerability and precipitating factors have been explored, the therapist should explore potential family maintaining factors. Various parental responses can have an impact on the continuation of obsessive compulsive symptoms. For example, parents who understandably become involved in their child’s rituals as a way of ‘helping them get them done more quickly’, or who give regular reassurance ‘to try and make them realise there is nothing to worry about’, or who try to clear their child’s path of potential triggers are all inadvertently keeping the problem going. Such responses fail to provide the young person with experiences that allow them to see that their problem is just worry (rather than real danger) and that their obsessions are just normal, insignificant intrusive thoughts (or urges, doubt and images) that they need do nothing about. Furthermore, these responses do not reinforce the young person’s own ability to cope with anxiety-provoking situations.
The therapist should also enquire about any parental beliefs relating to the nature and course of their child’s OCD; for example, whether they think
Cognitive behavioural assessment of OCD
37
their child is ‘going crazy’ or ‘just being manipulative and using their OCD to get away with things’. Parents sometimes get into the trap of viewing the OCD
as an essential rather than accidental feature of their child, which can have implications on their beliefs about the possibility of change. Whilst enquiring about parental beliefs and behaviours the therapist should consider that the parent’s own OCD or anxiety difficulties (if previously identified) may be validating their child’s symptoms through modelling. It is also important that the therapist undertakes sensitive enquiry about possible parental maintaining factors and normalises any beliefs or behaviours that are identified.
‘We often find that parents start to think and do all sorts of things that they are not sure are actually that helpful because living with a child with OCD is just so difficult. Some parents get involved in their child’s rituals or feel that they have to reassure them all the time because it is so hard watching their child suffer at the hands of OCD. Others get really frustrated and annoyed or feel that their child is using their OCD as an excuse for getting out of doing things. Others have given up believing that their child will ever get better because OCD has been around for so long. Do you ever find that you are thinking or doing things that you are not sure are actually helping the problem?’
The therapist should give special consideration to possible family and environmental factors that may be related to the onset and maintenance of the OCD.
Specific OCD symptomatology
Once potential family and developmental factors have been identified, assessment should focus on gaining information on the young person’s primary presenting difficulties. Diagnostic, symptom-based and diary measures are all essential but further idiosyncratic information should be gained via clinical interview. It is important to begin this part of the interview with open questions in order to gain a general description of the nature of the young person’s problem: for example, ‘Can you tell me about some of the difficulties you have been having recently?’ If the young person begins to divulge information that is not relevant to their OCD, it can be helpful to ask them to focus on a recent specific time when their OCD became problematic: for example, ‘I am particularly interested in any upsetting thoughts or pictures which have been going through your mind and anything you have had to do because of these thoughts and pictures. Can you tell me about a recent time when you were really bothered by one of these thoughts?’
Once the young person identifies a recent time when they have been bothered by their OCD the therapist should undertake a detailed analysis of 38
Gallop
any triggering stimuli (which can be internal) or situations; the precise form (i.e. thoughts, picture, urge, doubt) and content (e.g. contamination, harm, symmetry and order, etc.) of the obsessions and the precise nature of any covert (e.g. mental rituals) and overt (e.g. hand-washing, ordering, etc.) neutralising strategies. When asking about the young person’s compulsive behaviours it is important to ask about the precise way in which any compulsions brought about relief. The therapist should also enquire about the young person’s emotional reaction to the obsessions and any other cognitive or behavioural efforts (e.g. avoidance, looking out for danger, reassurance seeking, arguing back at the thought or trying to block the thought from their mind) that are made in an attempt to control the obsession and its associated distress.
After exploring the recent specific example the therapist should conduct a detailed investigation of all other obsessions and compulsions by asking the young person if they are bothered by any other thoughts or things that they have to do. It can be helpful to give the young person examples of other obsessions and compulsions that are commonly seen and then to ask them if any of the examples are relevant to them. It is also helpful to identify the young person’s primary obsessions and compulsions by enquiring about frequency, duration and associated distress. When asking about the levels of distress, it is important to ask not only about distress associated with carrying out compulsions but also any distress experienced by the young person if they are prevented from completing their rituals. Levels of interference and any additional factors that lessen or worsen symptoms should also be noted.
Once the young person’s current obsessive compulsive symptoms have been explored, the therapist should ask about the history of the young person’s OCD. It is useful to enquire about the initial onset of their symptoms and any potential personal triggering events that have not already been covered in the family interview. Childhood OCD tends to fluctuate over time and it is therefore important to enquire about times when the young person’s symptoms have waxed and waned and any ideas they have about why these changes occurred. It is also important to note any changes in the form and content of their obsessions or compulsions given the ‘contagious’ nature of OCD.
The young person’s current obsessive compulsive symptoms should be identified by reviewing a recent occurrence of their OCD and then via the detailed investigation of possible obsessions and compulsions.
Cognitive appraisals and underlying beliefs
The cognitive behavioural theory views OCD as resulting from assumptions or beliefs that give rise to cognitive biases and faulty appraisals. Given that
Cognitive behavioural assessment of OCD
39
most adults experience intrusive thoughts similar in content to those reported by individuals with OCD (Salkovskis and Harrison, 1984), it is hypothesised that it is the appraisal (i.e. the expectation, interpretation or evaluation) of intrusive thoughts rather than the thoughts themselves that is problematic and implicit in the development and maintenance of OCD
(Salkovskis
et al.
, 2000). There is preliminary support for a downward extension of the beliefs and cognitive appraisals held in adult models of OCD to children (e.g. Barrett and Healy, 2003; Libby
et al.
, 2004).
When conducting the assessment, the therapist should therefore enquire about relevant beliefs and appraisals associated with the young person’s obsessions and compulsions. Detailed questioning around the young person’s interpretations of their obsessions and compulsions is required by focusing on a recent specific example of when their OCD bothered them.
Once the young person has been able to identify their intrusion, the therapist should ask what interpretation they made, for example, ‘After you had that thought, what did it mean to you? What was the worst thing that could have happened and why would that have been so awful?’ It can be helpful at this stage to offer examples or common misinterpretations: ‘Sometimes young people think that because they have had this thought, then it will come true. Others think that unless they do something to prevent it something really awful will happen and it will be their fault. Others still think that unless they do something to make themselves feel better they will lose control or go crazy and that the fact that they’ve had this thought means something bad about them. When you had your thought did it make you think any of these things?’
Information about the young person’s beliefs can be obtained via general questioning around how they tend to act or feel in day-to-day situations.
Figure 3.1 contains potential questions to guide the therapist when assessing for OCD-related beliefs.
The therapist should try to identify relevant beliefs and appraisals by asking the young person about their interpretations of their obsessions and compulsions and by examining how they tend to act or feel in day-to-day situations.
Assessing comorbidity
Given the highly comorbid nature of OCD, the therapist should be mindful of ascertaining whether OCD is the primary diagnosis and also of making accurate differential diagnosis. Structured diagnostic interviews can be extremely useful in guiding the therapist in making decisions about whether the diagnostic criteria of certain disorders are met. They can also help with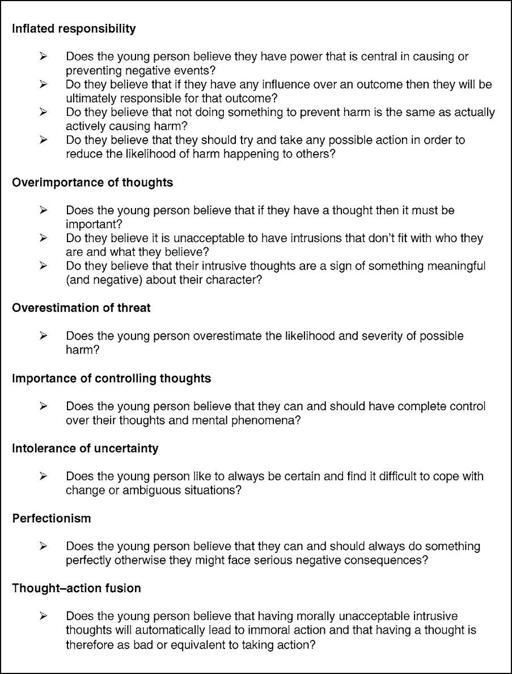
40
Gallop
Figure 3.1
Assessing for OCD-related beliefs
the issue of identifying what constitutes the primary disorder as they ask for both child and parental report on levels of interference and date of onset of individual disorders. However, due to the significant overlap between symptoms of OCD and other psychological disorders, childhood OCD can be difficult to diagnose and differential diagnosis can be challenging (Merlo
et al.
, 2005). When assessing for comorbidity the therapist should endeavour to distinguish obsessive compulsive symptoms from
Cognitive behavioural assessment of OCD
41
other clinical phenomena by considering both the common and distinct features of each disorder. Important commonalities and distinctions are highlighted below.
Separation anxiety disorder (SAD) and OCD share the common fear that harm may come to others and both may involve the young person seeking reassurance from parents and family members. However, what distinguishes SAD is that anxiety is limited only to separation from loved ones and no compulsions are undertaken to prevent harm. With generalised anxiety disorder (GAD) the themes are usually about everyday concerns (e.g. school and friendships and family members’ health) and are therefore distinguishable from OCD fears, which tend to be more unusual or ‘magical’
in nature. OCD fears can also be distinguished from the fears in social phobia and with specific phobias where they are limited to social evaluation/
situations and specific objects and situations respectively. Young people with OCD may suffer from panic symptoms due to the intense fear associated with the misinterpretation of their obsessions. However, in order for panic disorder to be diagnosed the young person has to experience repeated, unexpected panic attacks and have persistent anxiety about further impend-ing attacks.