Examination Medicine: A Guide to Physician Training (90 page)
Read Examination Medicine: A Guide to Physician Training Online
Authors: Nicholas J. Talley,Simon O’connor
Tags: #Medical, #Internal Medicine, #Diagnosis

FIGURE 16.65
(a) to (d) Osteoarthritis of the hands. T L Vincent, F E Watt. Rheumatology, part 1 of 2: osteoarthritis practice points,
Medicine
, 2009. 38(3):151–156, Fig 2.
FIGURE 16.71
X-ray of the hands of a patient with severe osteoarthritis. Note Heberden’s nodes and DIP joint involvement. Figure reproduced courtesy of The Canberra Hospital.
HINT
Severe osteoarthritis can cause hand deformity. Sometimes more than the DIP and PIP joints are involved, but these are usually the worst.
Destructive changes (especially shortening and telescoping of digits) and DIP disease suggests sero-negative arthropathy – look carefully for psoriasis.
FIGURE 16.67
X-ray of the hands showing advanced destructive changes in a patient with rheumatoid arthritis. Note ulnar deviation, Z deformity of the thumb, destruction of the PIP and MCP joints, and bone erosion. Figure reproduced courtesy of The Canberra Hospital.
Look carefully while doing your hand examination for any of these possibilities.
At the end, ask whether you may examine all the other joints that are likely to be involved and the other systems likely to be affected.
The knees
‘This 70-year-old man has had painful knees. Please examine him.’
Method
1.
Expose both knees and thighs fully and have the patient lie on his back.
2.
Look for quadriceps wasting and then over the knees for any skin abnormalities (scars or rashes), swelling and deformity. Synovial swelling is seen medial to the patella and in the suprapatellar area. Fixed flexion deformity must be assessed. This is looked for by inspecting the knee from the side (a space beneath the knee is seen).
3.
Feel the quadriceps for wasting.
4.
Ask about tenderness and palpate for warmth and synovitis over the knee joint.
5.
Examine for effusions – the patella tap (ballottement) is used to confirm a large effusion. The fluid from the suprapatellar bursa is pushed by the hand into the joint space by squeezing the lower part of the quadriceps and then pushing the patella downwards with the fingers. The patella will be ballottable if fluid is present under it. In patients with a smaller effusion, pressing over the lateral knee compartment may produce a noticeable medial bulge as a result of fluid displacement.
6.
Test flexion and extension passively and note the range of movement and the presence or absence of crepitus.
7.
Examine for fixed flexion deformity by gently extending the knee.
8.
Test the ligaments next. The lateral and medial collateral ligaments are tested by having the knee slightly flexed, holding the leg with the right hand and arm, steadying the thigh with the left hand and moving the leg laterally and medially. Movements of more than 5–10° are abnormal. The cruciate ligaments are tested by steadying the foot with your elbow and moving the leg anteriorly and posteriorly with the other hand. Again, laxity of more than 5–10° is abnormal.
9.
Use McMurray’s test for meniscal integrity. Hold the lower leg and foot, flex and extend the knee while internally and externally rotating the tibia. Pain or clicking is very suggestive of a meniscal tear.
10.
Ask the patient to stand up and examine for a Baker’s cyst, which is felt in the popliteal fossa and is more obvious when the knee is extended.
11.
Proceed then to examine other joints that may be involved or test function by asking the patient to walk.
HINT
The knees and other hinge joints are commonly affected in patients with arthritis secondary to haemophilia. The pattern of joint involvement and juxta-articular bony sclerosis on X-ray film help to distinguish this from rheumatoid arthritis involving the knees (see
Figs 16.72
and
16.73
).
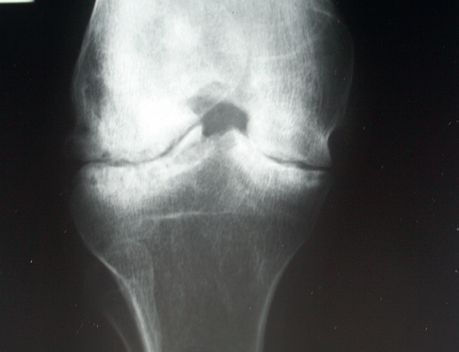
FIGURE 16.72
X-ray of the knee joint of a patient with arthritis secondary to haemophilia. Note loss of joint space. The juxta-articular aspects of the tibia and femur appear sclerotic, but the bones are generally osteoporotic. Figure reproduced courtesy of The Canberra Hospital.
FIGURE 16.73
X-ray of the knee of a patient with rheumatoid arthritis. Here there is more severe joint space loss. Figure reproduced courtesy of The Canberra Hospital.
The feet
‘This 50-year-old woman has painful feet. Please examine her (her feet).’
Method
1.
Start by inspecting the ankles. Look at the skin of the feet and toes (for scars, ulcers and rashes), and look for swelling, deformity and muscle wasting. Examine the midfoot and forefoot similarly. Deformities affecting the forefoot include hallux valgus and clawing and crowding of the toes (in rheumatoid arthritis). If pes cavus is present, consider a hereditary motor and sensory neuropathy.
2.
Note any psoriatic nail changes. Look at the transverse and longitudinal arches. Look for callus over the metatarsal heads, which occurs in subluxation. Note any obvious painless deformities or Charcot’s joints.
3.
Palpate, starting with the ankle, feeling for synovitis and effusion. Passive movement of the talar joints (dorsiflexion and plantarflexion) and subtalar joints (inversion and eversion) must be assessed. The best way to examine the subtalar and midtarsal joints is to fix the os calcaneus and ankle joint with the left hand while inverting and everting the midfoot with the right. Tenderness on movement is more important than range of movement. The midfoot (midtarsal joint) allows rotation of the forefoot on a fixed hindfoot. Squeeze the metatarsophalangeal joints for tenderness.
4.
Examining the individual toes is useful in seronegative spondyloarthropathies (a sausage-like swelling of the toe is characteristic in psoriatic arthritis).
5.
Feel the Achilles tendon for nodules and palpate the inferior aspect of the heel for tenderness (plantar fasciitis).
6.
Consider a neurological examination – test pinprick sensation and proprioception. Go on to examine other joints as appropriate.
X-rays of the feet are the most likely investigations that will be available (see
Figs 16.74
–
16.78
). Patients with rheumatoid arthritis can have involvement of the cervical spine, hips and shoulders, and X-rays of these may also be available.
FIGURE 16.74
(a) X-ray of the feet of a patient with early rheumatoid arthritis. Note the joint erosions and deformity of some of the MTP and PIP joints.
(b) X-ray of the ankles of a patient with rheumatoid arthritis. There is generalised loss of joint spaces, and early destructive changes are present. Figure reproduced courtesy of The Canberra Hospital.