Pediatric Primary Care Case Studies (121 page)
Read Pediatric Primary Care Case Studies Online
Authors: Catherine E. Burns,Beth Richardson,Cpnp Rn Dns Beth Richardson,Margaret Brady
Tags: #Medical, #Health Care Delivery, #Nursing, #Pediatric & Neonatal, #Pediatrics

• Is there a family history of asthma or hay fever?
• Has the rash ever been weeping or covered in an exudate?
• What type of soap is used in bathing and in laundry care?
• Has the mother been trying any home remedies on the rash?
• Has the child been seen by a physician in the past and treated for skin problems?
• How much sleep does the child get at night?
The mother responds that Anna is one of three children in the family. Her eldest daughter is on medication for asthma while the other child has intermittent seasonal allergies. Anna has had a history of some early childhood milk allergies that she seems to have outgrown. The mother indicates that she changed her daughter’s clothes from wool to cotton fiber when she discovered that her daughter’s scratching became worse in the wool clothing. During bathing, the mother uses Dove soap and has been applying Lubriderm cream after her daughter gets out of the bath. The rash persists despite the lotion treatment, and her daughter is getting only about 4–5 hours of sleep at night. The mother and her husband are getting less sleep also because they have to get up with their daughter in the night when she cannot sleep. This is beginning to cause some stress in the family. There have been no other medical visits or treatments.
Making the Diagnosis
The common conditions that should be considered in the differential diagnosis for atopic dermatitis are as follows:
• Classic atopic dermatitis
Infantile seborrheic dermatitis
Irritant or allergic contact dermatitis
Nutritional dermatitis; immunodeficiency
• Nummular dermatitis

Dry form:
Tinea corporis, psoriasis, pityriasis rosea

Wet form:
Impetigo, burns, allergic contact
• Dyshidrotic eczema
• Bullous impetigo
• Allergic bullous tinea
• Contact dermatitis
Reviewing the facts gained from the history and the correlating physical findings, you are assured that this child has atopic dermatitis. The patient has chronic scratching as well as a red erythematous rash on the flexor folds of her arms and knees with early lichenification. There is a history of asthma in the family and allergic rhinitis. The rash first appeared at age 1 year, and Anna has a mild to moderate case of atopic dermatitis.
Diagnostic tests are not indicated at this time because the child has mild involvement and the family is aware of the triggers for this disease and have already made changes to her clothing, bathing, and allergy exposure.
Management
Management of atopic dermatitis in children should follow a stepped approach, with treatment steps tailored to the severity of the eczema. Even when the eczema clears, emollients should always be used and should form the basis of
the management. Parents should be counseled on symptoms of atopic dermatitis flares, which include increased dryness, itching, redness, swelling, and general irritability, as well as how to treat the flares through a step-wise care plan (Barclay, 2008; Krakowski et al., 2008).
General Measures
All patients with atopic dermatitis, including children, have hyper-irritable skin. It is important to avoid irritants such as soaps, cleaning agents, detergents, heat, and wool clothing. Over-the-counter preparations such as Aquaphor, CeraVe, Eucerin, or Vaseline are helpful. Newer prescription emollients such as Epiceram or Hylira are also available. Barrier repair formulations have recently come on the market and include ceramide-based creams such as TriCeram, Impruv, TriXera, Nouriva Repair, and Stelatopia. Their drawback is expense, particularly when the medication is used to cover large areas of the body. Emollients should be applied twice daily and immediately after bathing (Darsow et al., 2005).
Bathing remains somewhat controversial. On the one hand, bathing promotes skin hydration, cleansing, and absorption of topical therapies. On the other hand, bathing can dry the skin and disrupt the stratum corneum barrier during evaporation if emollients are not immediately used to maximize moisture retention (Krakowski et al., 2008). Soaps such as Eucerin, Dove, Aveeno, and Alpha Keri may provide benefit.
Treatment of the pruritis in children is also extremely important because sleep deprivation becomes a factor parents have to deal with frequently. General measures may include cooling the skin with cool wraps or cool baths. Moisturizing and minimizing itching are essential. Oral antihistamines have not been shown to be very effective at reducing itch, but sedating antihistamines may promote night-time sleep.
Topical Corticosteroids
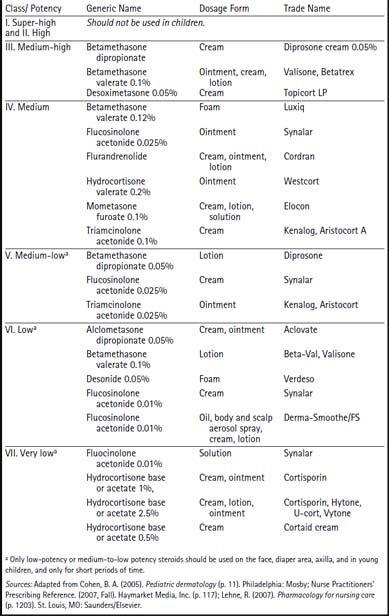
Topical corticosteroids are divided into classes based on their potency. Class 1 is the most potent of steroids whereas class 7 is the least potent (
Table 30-1
). Class 1–5 steroids are not to be used in areas of thinner skin including the eyelids, face, mucous membranes, genitalia, and intertriginous areas because those areas have increased likelihood of transepidermal corticosteroid absorption (Leung et al., 2004). Higher potency steroids should be avoided in children (Paller et al., 2005).
Topical steroids should be used for only a few weeks in a continuous fashion and then tapered as soon as symptoms improve. It is preferable to use low-potency steroids for maintenance therapy and mid- to high-potency steroids for flares (Leung et al., 2004). Traditional vehicle choices are ointments for dry skin, creams or lotions for moist skin, lotions or foams for hair-bearing areas, and lotions for facial skin in teens. Local side effects of steroids include striae, telangiectiasis, skin atrophy, dyspigmentation, and acneiform eruptions.
Table 30–1 Common Topical Corticosteroids by Potency
Topical Calcineurin Inhibitor (TCIs)
This class of medications exhibits a potent anti-inflammatory effect without the immune suppression caused by corticosteroids. Pimecrolimus (Elidel) and tacrolimus (Protopic) are safe products in children after the age of 2 years. Pimecrolimus is effective in treating mild to moderate atopic dermatitis whereas tacrolimus is more often used to treat moderate to severe atopic dermatitis. Both are applied two times a day and can be used concomitantly with topical steroids. In addition, both can be used in areas of thinner skin without the risk of skin atrophy and striae (Peterson & Chen, 2006). These agents inhibit the phosphatase activity of calcineurin, thereby preventing the expression of a number of proinflammatory cytokines (interleukin [IL]-2, IL-3, IL-4, IL-5, granulocyte-macrophage colony-stimulating factor, tumor necrosis factor-alpha, and interferon-gamma), which play significant roles in the pathophysiology of atopic dermatitis (Nghiem, Peterson, & Langley, 2002). These agents have decided advantages over topical corticosteroids because they can be used safely on the face and in intertriginous areas without causing skin atrophy, striae, hypopigmentation, or hypothalamic-pituitary-adrenal (HPA) axis suppression.
Topical calcineurin inhibitors can be used safely around the eyes of atopic dermatitis patients without concern for increasing intraocular pressure or contributing to cataract formation (Tharp, 2005).
Systemic Therapy
Systemic steroids may be employed for a short period of time to treat severe atopic dermatitis. However, concerns over side effects and a rebound effect that may occur after discontinuation limit their use (Abramovits, 2005). In severe recalcitrant atopic dermatitis immunomodulators (cyclosporine, azathioprine, mycophenolate mofetil) may also be needed, but it is imperative that these patients be followed closely to detect any side effects. These types of medications should not be used long term (Paller et al., 2005).