Pediatric Primary Care Case Studies (11 page)
Read Pediatric Primary Care Case Studies Online
Authors: Catherine E. Burns,Beth Richardson,Cpnp Rn Dns Beth Richardson,Margaret Brady
Tags: #Medical, #Health Care Delivery, #Nursing, #Pediatric & Neonatal, #Pediatrics

• Recheck the child’s head circumference. Twenty-five percent of autistic children exhibit macrocephaly.
• Despite the mother’s report and your documentation of normal tympanic membranes, a formal audiological evaluation is warranted to rule out a hearing problem (Filipek et al., 2000).
• Lead testing is indicated if not done previously (Filipek et al.).
• Various screening tools are available to assist the clinician in further evaluation of the child suspected of having an autistic spectrum disorder, such as the Pervasive Developmental Disorder Screening Test (PDDST-II) (Siegel, 2004a, 2004b), Checklist for Autism in Toddlers (CHAT) (Baird et al., 2000), and the Modified Checklist for Autism in Toddlers (M-CHAT) (Robins, Fein, Barton, & Green, 2001). These questionnaires are designed to be completed by the parent and subsequently scored by the clinician. The CHAT includes additional clinical observation questions. In the M-CHAT (
Figure 3-2
), critical items indicative of autism include:
Lack of response when called by name
Lack of imitation/reciprocation
Failure to “follow a point”
Lack of pointing to indicate interest
Lack of interest in other children
Lack of bringing objects over to parent to “show”
What additional diagnostic testing might be considered?
Although routine screening for ASDs in the primary care setting is based on clinical observation, laboratory investigation may be warranted given the child’s presentation. More sophisticated testing, if indicated, is usually initiated by a pediatric specialist (e.g., a pediatric neurologist, psychiatrist, geneticist, or developmental pediatrician) (Filipek et al., 2000).
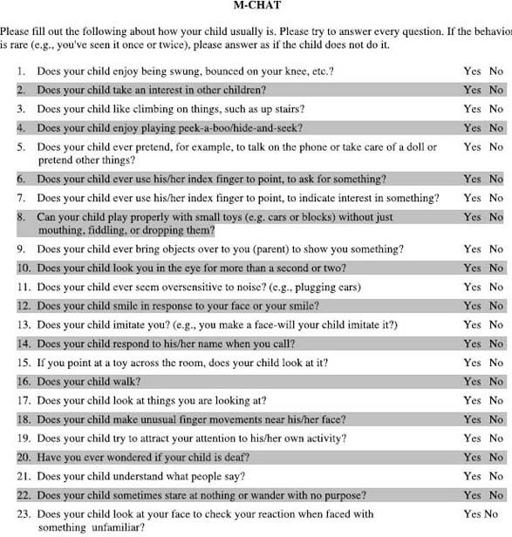
Source: ©
1999 Diane Robins, Deborah Fein, & Marianne Barton. Used with permission.
Please refer to Robins, D., Fein, D., Barton, M., & Green, J. (2001). The Modified Checklist for Autism in Toddlers: An initial study investigating the early detection of austism and pervasive developmental disorders.
Journal of Autism and Developmental Disorder, 31
(2), 131–144.
Note
. The Modified Checklist for Autism in Toddlers (M-CHAT) and supplemental materials are available for free download for clinical research and educational purposes. There are two authorized Web sites that these materials can be downloaded from:
www.firstsigns.org
and
www2.gsu.edu/~wwwpsy/faculty/robins.htm
. Users should be aware that the M-CHAT continues to be studied and may be revised in the future. Any revisions will be posted to the two Web sites noted above. The M-CHAT must be used in its entirety. There is no evidence that using a subset of items will be valid.
Figure 3-2 Modified Checklist for Autism in Toddlers (M-CHAT).
Were James to meet the criteria for global developmental delays and mental retardation (GDD/MR), high-resolution chromosome analysis and DNA for fragile X testing would be indicated. Seven to eight percent of children with ASD test positive for fragile X (Muhle et al., 2004).
In children with cyclic vomiting, unusual odor, regression of skills, or dysmorphic features, selective metabolic testing may be considered. In the absence of seizure activity or focal neurological signs, routine EEG and neuroimaging are not indicated.
Many times children suspected of having an ASD are referred to a pediatric developmental specialist for further evaluation.
Management
You express your concerns about James’s development to Ms. Jones and suggest that further testing be done. She concurs.
Diagnostic and Intervention Plan
The results of laboratory testing and audiological screening are within normal limits. You refer James to a developmental pediatrician. As part of his evaluation, a Childhood Autism Rating Scale (CARS) (Schopler, Reichler, DeVellis, & Daly, 1980) is administered. Numerical values are assigned given the child’s performance on this 15-item assessment tool. A score above 30 on the CARS is suggestive of an autistic spectrum disorder. On the basis of the specialist’s assessment, James’s profile falls into the category of autistic spectrum, meeting the criteria for autism disorder. Placement in an early intervention program specializing in children with autistic spectrum disorders is recommended. Fortunately, the family’s local school district has an excellent center that specializes in children with this disorder.
Educational interventions form the basis for management of children with ASDs. The sooner the intervention is initiated, the better the outcome. Children with ASDs should be actively engaged in an intervention program at least 25 hours per week throughout the calendar year (Myers & Johnson, 2007).
Specific methodologic programs include Applied Behavior Analysis (ABA), highly structured comprehensive early intervention programs, and functional behavior analysis. ABA methods are designed to shape desirable adaptive behaviors, and their effectiveness has been well documented (Barbaresi et al., 2006; Myers & Johnson, 2007). The Treatment and Education of Autistic and Related Communication-Handicapped Children (TEACCH) program emphasizes structured teaching and environmental modification to improve skills of individuals with ASDs.
Other appropriate interventions include speech and language therapy, social skills instruction, and occupational therapy. Primary care providers play
a vital role in advocating these services for the child with an ASD as well as the child’s need for continuing participation in programs for autistic children throughout childhood.
