Pediatric Examination and Board Review (75 page)
Read Pediatric Examination and Board Review Online
Authors: Robert Daum,Jason Canel

10.
(D)
Most pediatric drug suspensions contain sucrose (a disaccharide that contains glucose and fructose) and can induce symptoms in patients with hereditary fructose intolerance. Fructoaldolase levels are measured in liver tissue, not blood. The metabolic consequences of the disease are secondary to accumulation of fructose-1-phosphate (see
Figure 46-3
). In addition to the metabolic consequences, the child may develop hepatic failure. Therefore, each child should have a prothrombin time test and an NH
3
level measured.
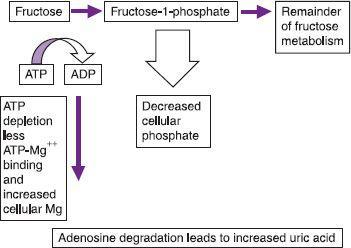
FIGURE 46-3.
Fructose metabolism.
11.
(E)
It is impossible to distinguish between biliary atresia and neonatal hepatitis based on these laboratory results.
12.
(B)
Hepatobiliary scintigraphy can (under the right conditions) distinguish between biliary atresia and neonatal hepatitis. In neonatal hepatitis, dye is excreted from the liver into the gut; in biliary atresia it is not. The test, however, has significant limitations. It is most reliable when the patient has been pretreated with phenobarbital for 5 days to induce biliary flow. Even with pretreatment, the liver often does not excrete bile in the presence of significant cholestasis. If the serum bilirubin level is more than 10 mg/dL, failure to excrete is almost universal and this test is unreliable and unhelpful. Because of the issues of patient size, ERCP is very difficult to perform in a 1-month-old. Very few gastroenterologists are skilled enough to do a successful ERCP at this age. If there is no gallbladder visualized on an ultrasound, that finding is consistent with biliary atresia but not diagnostic. Liver biopsy will best distinguish between these 2 diseases and provide an accurate and expeditious diagnosis. Percutaneous liver biopsy can safely be performed by many gastroenterologists and radiologists.
13.
(B)
See below.
14.
(D)
The procedure to correct biliary atresia is known as a Kasai procedure. In the Kasai procedure, an intrahepatic bile duct is connected directly to a loop of bowel to provide bile drainage and delay hepatic damage. The likelihood of success of the Kasai decreases dramatically when performed after 8 weeks of age. Because of this, making a definitive diagnosis and instituting therapy quickly is vital. Without a successful Kasai procedure, the patient will be committed to an early liver transplant. Because of the difficulty in obtaining ideally size-matched organs in a very young patient, this is not ideal.
15.
(D)
Neonatal hepatitis resolves in most patients. This hepatitis is not infectious, and antiviral medications are not indicated. Ten percent of patients develop end-stage liver disease and require a liver transplant. Any pediatric patient with cholestasis requires medical support for the cholestasis.
16.
(B)
Patients with cholestasis have a decreased ability to absorb fats (nutritional support) and fatsoluble vitamins (A, D, E, and K). Ursodiol protects the liver during cholestatic injury. Pruritus can also develop in cholestatic patients and can be treated with antihistamines, rifampin, or naltrexone.
17.
(E)
In newborns, the likely diagnosis for cholestatic liver disease is an infectious etiology. There are 2 types of biliary atresia. The most common was detailed in previous discussions, but there is also a rare neonatal form that is more likely associated with other congenital anomalies and can present in the first week of life. Ornithine transcarbamylase (OTC) deficiency is a urea cycle defect and would present with hyperammonemia and alteration in mental status.
18.
(A)
The laboratory data reveal a child with liver failure and disseminated intravascular coagulopathy (DIC). Bacterial infections can cause DIC and should be considered. Viral infections can cause hepatosplenomegaly and liver failure. With neonatal hemochromatosis infants are born with cirrhosis (small liver and splenomegaly) and liver failure. The diagnosis is made by demonstration of iron deposits in the pancreas on MRI. Liver biopsy in this child would be extremely dangerous and should be avoided if possible.
 S
S
UGGESTED
R
EADING
Bezzerra JA, Balistreri W. Cholestatic syndromes in infancy and childhood.
Semin Gastrointest Dis.
2001;12(2):54-65.
McKiernan PJ. Neonatal cholestasis.
Semin Neonatol.
2002;7(2):153-165.
CASE 47: AN 11-YEAR-OLD WITH CRAMPING ABDOMINAL PAIN
An 11-year-old girl is brought to your office with a complaint of periumbilical abdominal pain for 5 weeks. The pain is increased when the patient eats and relieved by stooling. The pain has awakened her from sleep several times. Ranitidine did not improve her symptoms. She denies melena or weight loss, but she has seen blood in her stool.
On physical examination she is a tired-appearing young lady whose weight is 34 kg (25%) and her height is 134 cm (10-25%). She has nonicteric sclera and a moist oropharynx. Her abdomen is nondistended with positive bowel sounds. There is no hepatosplenomegaly or masses. There is diffuse suprapubic tenderness. Rectal examination demonstrates normal sphincter tone and heme-positive stool.
SELECT THE ONE BEST ANSWER
1.
Possible diagnoses for this child include
(A) inflammatory bowel disease
(B) infectious colitis
(C) irritable bowel syndrome
(D) peptic ulcer disease
(E) all of the above
2.
Stool studies that are ordered should include
(A) search for fecal-reducing substances
(B) a bacterial culture
(C) a stool fungal culture
(D) ova and parasite examination
(E) none of the tests are likely to be useful
3.
Likely stool pathogens include
(A)
Campylobacter jejuni
(B)
Yersinia enterocolitica
(C)
E coli
O157:H7
(D)
Clostridium difficile
(E) all of the above
4.
If the child’s CBC demonstrated a platelet count of 50,000, the next laboratory study(ies) you should order is/are
(A) erythrocyte sedimentation rate
(B) hepatic function panel
(C) serum creatinine
(D) PT
(E) all of the above
5.
If the stool cultures were negative, the patient’s weight was 23 kg (<5th percentile), and the height was 123 cm (<5th percentile), your next step would be to check
(A) CBC, sedimentation rate, and C-reactive protein
(B) CBC, PT, bleeding time
(C) CBC, differential, and platelet count
(D) viral stool cultures
(E) antigliadin immunoglobulin (Ig)G antibodies
6.
Below are the laboratory values for the patient in question 5
| Hemoglobin | 8.5 g/dL |
| Platelets | 550,000/mm 3 |
| Mean corpuscular | 75 fL |
| volume (MCV) | |
| Sedimentation rate | 58 mm/s |
| Albumin | 2.8 g/dL |
| Gamma-glutamyl | 300 IU/L |
| transpeptidase (GGTP) | |
| Alkaline phosphatase | 550 IU/L |
The first radiology study you should order is
(A) abdominal radiograph
(B) barium enema
(C) upper gastrointestinal (GI) series with small bowel follow-through
(D) upper GI series without small bowel followthrough
(E) abdominal ultrasound
7.
The findings you might expect on the study ordered in question 6 include
(A) bowel wall thickening in the ileum
(B) strictures in the jejunum
(C) fistulas
(D) delayed transit to the colon
(E) all of the above
8.
What additional symptoms might your patient have suffered?
(A) early satiety
(B) right upper quadrant (RUQ) pain
(C) perianal abscess
(D) skin rash