Pediatric Examination and Board Review (224 page)
Read Pediatric Examination and Board Review Online
Authors: Robert Daum,Jason Canel

SELECT THE ONE BEST ANSWER
1.
Based on the clinical history, this child most likely has which of the following diagnoses?
(A) depression
(B) absence seizures
(C) complex partial seizures
(D) juvenile myoclonic epilepsy
(E) attention deficit disorder
2.
To establish the diagnosis in the clinic, which of the following actions would be the most helpful?
(A) assessment of risk factors for depression
(B) Connor scales
(C) visual screening
(D) hyperventilation
(E) none of the above
3.
Which of the following diagnostic studies would be the most helpful in establishing the diagnosis?
(A) electroencephalogram (EEG) with hyperventilation and photic stimulation
(B) magnetic resonance imaging (MRI) of the brain, with and without contrast
(C) urine toxicology screen
(D) electrolytes
(E) polysomnogram
4.
The drug treatment of choice for this patient would be which of the following medications?
(A) lamotrigine
(B) ethosuximide
(C) carbamazepine
(D) methylphenidate
(E) fluoxetine
5.
A child presents to your office with the chief complaint of staring lasting up to 80 seconds. During the event, the child exhibits lip smacking and is unresponsive to verbal and tactile stimuli. The child states that on occasion a “strange feeling” precedes the episodes. He has had one generalized tonic-clonic seizure observed by the school nurse. The child most likely has which of the following diagnoses?
(A) migraines with aura
(B) complex partial seizures
(C) absence seizures
(D) juvenile myoclonic epilepsy
(E) depression
6.
A 5-year-old girl comes to your office because she has started to lose the ability to speak. Her mother states that she was born full term and developed normally, speaking in full sentences by 3 years of age. She has a normal physical examination, including her head circumference that has been at the 50th percentile. A head computed tomography (CT) without contrast was within normal limits. Which of the following studies is most likely to yield the diagnosis?
(A) MRI of the brain with and without contrast
(B) lumbar puncture
(C) 24-hour long-term video EEG monitoring
(D) methyl CpG-binding protein 2 (MECP2) gene mutation analysis
(E) hearing test
7.
A 15-year-old boy with a history of complex partial seizures recently moves into your practice area. He comes into your office for a general physical examination. During the visit, he states he has been seizure-free for approximately 2
1
/
2
years. His spells consisted of staring with automatisms, but occasionally they would progress to generalized tonic-clonic seizures. Because he is concerned about driving next year, he asks you when he can go off his medication. He is currently treated with carbamazepine. The most appropriate response would be which of the following?
(A) “let’s obtain an EEG. If that test is normal, there is an approximately 70% chance you will be seizure-free upon weaning off the carbamazepine”
(B) “never; epilepsy is a lifelong condition”
(C) “children with complex partial seizures need to be seizure-free for at least 5 years before a decision can be made”
(D) “it all depends on the epilepsy syndrome or type; complex partial seizures seldom go into remission”
(E) none of the above
8.
Which of the following antiepileptic drugs are generally considered the first- and second-line therapies for neonatal seizures?
(A) diazepam and phenobarbital
(B) phenobarbital and phenytoin
(C) phenytoin and midazolam
(D) phenobarbital and lorazepam
(E) phenobarbital and valproic acid
9.
Which of the following is the most common form of childhood seizures?
(A) complex partial seizures
(B) absence seizures
(C) infantile spasms
(D) benign rolandic epilepsy
(E) febrile seizures
10.
A child with a 2-year history of epilepsy has been seizure free on his current antiepileptic regimen for 18 months. Recently, he was diagnosed with attention deficit hyperactivity disorder (ADHD). He was started on methylphenidate and a few days later experienced a complex partial seizure. The most likely explanation for this breakthrough seizure is which of the following?
(A) the child has developed a new seizure type
(B) the child has stopped taking his antiepileptic medications
(C) the child is now depressed regarding the new diagnosis
(D) the event represents a pseudoseizure
(E) methylphenidate can lower the seizure threshold
11.
Which of the following statements is not true about febrile seizures?
(A) a febrile seizure is considered “complex” if it is prolonged, focal, or occurs multiple times per febrile illness
(B) a family history of febrile seizures in a first- or second-degree relative is a risk factor for the development of febrile seizures
(C) developmental delay is a risk factor for the development of a first febrile seizure
(D) up to 10% of patients with febrile seizures develop epilepsy
(E) carbamazepine and phenytoin are equally effective in the treatment of febrile seizures should one consider treatment
12.
Which of the following are causes of neonatal seizures?
(A) a hypoxic-ischemic episode
(B) metabolic abnormalities
(C) infection
(D) inborn errors of metabolism
(E) all of the above
MATCH EACH OF THE FOLLOWING ANTIEPILEPTIC DRUGS WITH ITS COMMONLY REPORTED SIDE EFFECT
13.
lamotrigine (A) gingival hyperplasia
14.
valproic acid (B) Stevens-Johnson syndrome
15.
phenytoin (C) hepatotoxicity
16.
carbamazepine (D) weight loss
17.
phenobarbital (E) agranulocytosis
18.
topiramate (F) hyperactivity
ANSWERS
1.
(B)
This patient most likely has absence seizures (petit mal). Absence seizures are relatively uncommon, accounting for less than 10% of all seizure types. They tend to be more common in females than males. The average age of onset is approximately 4 years, and they are rarely seen before the age of 2 years. In typical absence seizures, patients exhibit brief (<30 seconds) staring spells; however, motor, behavioral, and autonomic phenomena are frequently observed. The child can have multiple spells per day. Automatisms, such as chewing, grimacing, or lip licking, may be observed. They are never associated with an aura, bowel or bladder incontinence, or postictal impairment. Most children with typical absence seizures have normal intelligence and a normal physical examination. There is a strong genetic predisposition. An EEG typically demonstrates generalized 3-Hz spikewave activity. The prognosis of typical absence seizures is favorable with approximately 80% achieving remission by 10-11 years of age. Atypical absence seizures are similar to typical absence seizures but are more likely to have diminished postural tone and tonic or myoclonic activity as part of their initial clinical presentation. Automatisms are less likely. Many children go on to develop Lennox-Gastaut syndrome. The EEG demonstrates asymmetric less than 2.5-Hz spike-wave activity with multifocal spikes and sharp waves. In contrast, complex partial seizures tend to last much longer (>1 minute on average), are frequently associated with an aura, and can be followed by a postictal state. The EEG usually demonstrates rhythmic focal spikes or sharp waves over the temporal or frontal regions during a seizure. Juvenile myoclonic epilepsy (JME) typically occurs between the ages of 12 and 18 years. Children as young as 8 years have been reported to develop JME. JME is a familial, generalized seizure disorder in which patients demonstrate jerks of the shoulders and arms, typically occurring shortly after awakening. Loss of consciousness is seldom noticeable. Many of these patients respond to valproic acid.
2.
(D)
Hyperventilation is a strong activator of typical absence seizures. The child is asked to hyperventilate for 3-5 minutes, during which a seizure is induced. Photic stimulation is also used to induce generalized seizure disorders but does not appear to be as effective an activator in typical absence seizures as hyperventilation. Connor scales are used to screen for attention deficit disorder.
3.
(A)
The differential diagnosis of absence seizures includes complex partial seizures, daydreaming, and pseudoseizures. The most effective way of establishing the classification of a seizure or establishing a diagnosis is to capture a spell while performing an EEG. In this case, hyperventilation can be used to precipitate a seizure, enabling the physician to capture the spell while recording. Bilateral, synchronous 3-Hz spike-wave activity would confirm the diagnosis of typical absence seizure (see
Figure 131-1
). In complex partial seizures, one may observe intermittent spikes or sharp waves over the temporal or frontal regions during the interictal (between seizures) stage, and rhythmic activity over these regions during the seizure. The EEG should be normal in daydreaming and pseudoseizures. MRI of the brain, urine toxicology, and electrolyte analysis can be important in the diagnosis and management of seizures, but given the clinical history, an EEG with hyperventilation has the highest yield. The brain MRI, urine toxicity screen, and electrolytes are normal in typical absence seizures.
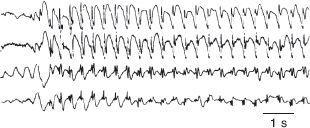
FIGURE 131-1
.
Absence seizures. Record of four cortical EEG leads from a 6-year-old boy who, during the recording, had one of his “blank spells” in which he was transiently unaware of his surroundings and blinked his eyelids. Time is indicated by the horizontal calibration line. (1 s = 1 second). (Reproduced, with permission, from Waxman SG. Clinical Neuroanatomy, 25th ed. New York: McGraw-Hill; 2003.)
4.
(B)
Three drugs are primarily used in the treatment of absence seizures: ethosuximide, valproic acid, and lamotrigine. For typical absence seizures, most neurologists would start therapy with ethosuximide given its side-effect profile compared with that of valproic acid. It is not useful for patients who have generalized tonic-clonic seizures with their absence seizures. In this case, valproic acid is preferred. Carbamazepine is used in the treatment of complex partial seizures. In primary generalized seizure disorders, such as absence seizures, it may make the patient worse. Methylphenidate is used in the treatment of ADHD; fluoxetine is used to treat anxiety, depression, and obsessive-compulsive disorders (OCDs).