Pediatric Examination and Board Review (134 page)
Read Pediatric Examination and Board Review Online
Authors: Robert Daum,Jason Canel

(B) physeal injury
(C) meniscal tear
(D) cruciate ligament injury
(E) tibial tubercle avulsion
11.
A 12-year-old girl comes to the emergency department after falling while playing basketball. Her knee is painful and swollen and she is unable to bear weight. Which study below would be the least helpful in initial diagnosis of a physeal injury?
(A) plain radiographs including AP, lateral, notch, and sunrise view
(B) CT scan
(C) MRI scan
(D) bone scan
(E) all are equally sensitive and specific to clarify the cause of a physeal injury
12.
Which of the following conditions is the least common cause of knee pain in adolescent females?
(A) patellar dislocation
(B) osteochondritis dissecans
(C) patellofemoral pain
(D) ACL injury
(E) meniscal injury
13.
An 11-year-old boy presents to the emergency department complaining of 4 weeks of localized pain below the knee. On examination the child is noted to have proximal tibial tuberosity tenderness. What is this child’s most likely diagnosis?
(A) patellofemoral pain
(B) Osgood-Schlatter disease
(C) plica band syndrome
(D) chronic MCL sprain
(E) iliotibial band syndrome
14.
Which of the following physical examination findings is not associated with an increased risk of patellofemoral pain?
(A) genu valgum
(B) pes planovalgus foot deformity
(C) Q angle of 15 degrees
(D) weak quadriceps muscles
(E) patellar hypermobility
15.
Which of the following activities is least associated with increased stress on the patellofemoral joint?
(A) jumping
(B) squatting
(C) prolonged sitting
(D) stair climbing
(E) straight leg raises
16.
A 15-year-old obese boy presents to the pediatric emergency department complaining of right hip pain during ambulation for 1 week. He denies trauma. On examination, he is noted to have a shortened right leg that is externally rotated and adducted. Before getting X-rays on her child, the mother wants to know her child’s most likely diagnosis
(A) femur fracture
(B) Legg-Calvé-Perthes disease
(C) toxic synovitis
(D) slipped capital femoral epiphysis
(E) congenital hip dislocation
17.
A 7-year-old is brought to the emergency department for a limp of 1 month duration and right hip pain. The mother states that the child fell off his bike 2 months ago. He had an evaluation at the time of the initial injury including X-rays of his hips that were normal. On examination, the child has a limited range of motion of the right hip due to pain at the joint. What do you expect to see when you repeat the hip radiographs?
(A) distal femur fracture
(B) femoral head fracture
(C) dislocation of the femoral head
(D) displacement of the epiphysis downward and posterior
(E) widened joint space between the femoral head and the acetabulum
ANSWERS
1.
(A)
The best initial treatment for an injured knee is ice applied to the swollen and painful area for approximately 20 minutes. It is appropriate to follow the general RICE (rest, ice, compression, elevation) principles for acute injury treatment. However, in the provided choices for an acute knee injury, one should not attempt to “force” the knee into extension because there may be mechanical limitations, such as torn tissue or extreme swelling that prevent the knee from reaching full extension. The knee joint has maximal space to accommodate swelling at approximately 30 degrees of flexion. Weight bearing should be as tolerated and, in this setting, keeping the athlete non-weight-bearing until a full examination is performed is appropriate. Although immediate use of ibuprofen or another NSAID may be helpful for pain, it is unlikely to have any immediate effect on the posttraumatic inflammatory response. Urgent treatment is prudent in the setting of sports-related knee injuries. In the absence of gross deformity or neurovascular compromise, emergent transport is unnecessary.
2.
(C)
A noncontact deceleration injury to the knee joint resulting in a painful “pop,” immediate swelling, and an inability to fully bear weight following the injury is an ACL tear approximately 85% of the time in a skeletally mature patient.
3.
(D)
The maneuver most helpful to confirm your diagnosis is the Lachman test performed at 30 degrees of flexion. The Lachman test is performed by using one hand to stabilize the femur while the examiner’s opposite hand is placed around the leg at the level of the tibial tubercle and an attempt is made to anteriorly translocate the tibia forward. The Lachman test is more clinically sensitive at diagnosing ACL tears than an anterior drawer test performed at 90 degrees of knee flexion (see
Figure 79-1
). In that instance, it is more common to find patients guarding or reflexively tightening their hamstring muscles; this results in a false-negative drawer test with decreased anterior translation. The McMurray test is performed with the patient lying supine. The examiner places one hand anteriorly on the joint lines and then proceeds to cup the heel with the opposite hand and begins to flex and extend the knee while simultaneously internally and externally rotating the tibia on the femur. The test is positive, indicating a torn meniscus, if a painful click is felt.
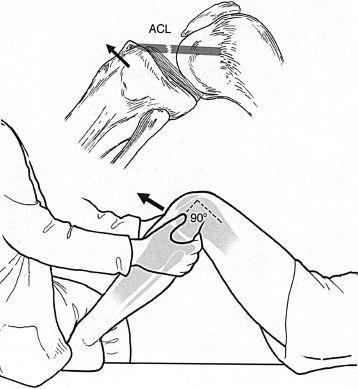
FIGURE 79-1.
Anterior drawer test. (Reproduced, with permission, from Imboden J, Hellmann DB, Stone JH. Current Rheumatology Diagnosis & Treatment, 2nd ed. New York: McGraw-Hill; Fig. 12-3.)
4.
(B)
Inflammation is both an acute and chronic response to trauma, infection, and systemic autoimmune disease. In the acute phase, inflammation may be a healthy, self-limiting response; however, in the chronic phase it is often destructive, such as in the setting of arthritis and articular cartilage destruction. Corticosteroids affect inflammation by inhibiting leukotriene production but also by inhibiting prostaglandin synthesis via the phospholipase A2 pathway.
5.
(E)
In the setting of traumatic knee injuries there is no role for acute corticosteroid injections and no significant therapeutic role for knee joint aspiration. If a joint aspiration is performed, the hemarthrosis tends to reaccumulate quickly, thus limiting the effectiveness of the therapeutic aspiration. An ACE wrap is a relatively ineffective way to provide support and compression if a more supportive knee brace is available. Knee immobilizers that do not allow for motion of the joint are acceptable alternatives initially, but their use should be limited to a few days, and active range of motion should be encouraged within the limits of pain.
6.
(D)
Although plain radiographs of the knee are an appropriate initial study, a noninfused MRI of the left knee is helpful in diagnosing ligamentous injuries of the knee, as well as diagnosing other associated intra-articular injuries, such as meniscal tears. Some might argue that no imaging study is needed in the case described because the diagnosis is clinically apparent; however MRIs are helpful to look for associated injuries such as collateral ligament, meniscal, and articular cartilage injuries. MRIs are generally recommended as part of the evaluation for an internal derangement of the knee. An MRI can be done as an outpatient in preparation for orthopedic follow-up care.
7.
(D)
ACL injuries usually result in complete ligament tears either midsubstance or from the proximal attachment on the posterior femur. The injured ligament usually retracts and loses proper anatomic positioning, thereby preventing any reasonable chance of healing with conservative management. Although bracing and physical therapy are important adjunctive treatments to decrease pain and improve strength and function, both pre- and post-surgery, the definitive treatment is an ACL reconstruction using a graft. Attempts to repair torn ACLs surgically have resulted in high failure rates and complications; therefore, in general, a surgical reconstruction is the preferred treatment of choice.
8.
(D)
Given the above information, your examination suggests ACL and meniscus injury resulting in signs of internal derangement. Bucket handle meniscal tears are most likely to result in a mechanical block in knee joint range of motion (see
Figure 79-2
). An MCL injury should be associated with pain to palpation over this extra-articular structure and increased laxity with valgus testing.
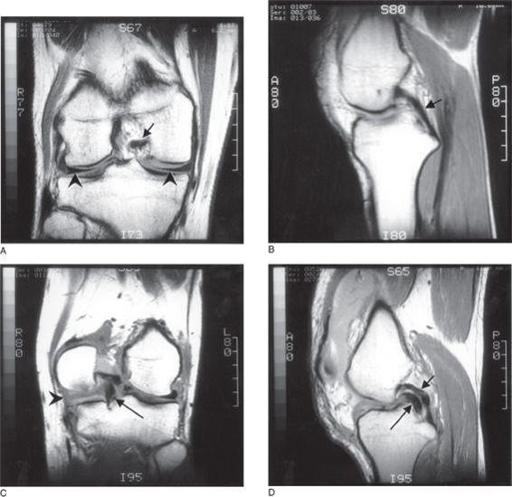
FIGURE 79-2.
Bucket-handle meniscal tear.
A.
Normal medial and lateral menisci and
B.
normal posterior cruciate ligament in the intercondylar notch as demonstrated on magnetic resonance proton-density (partial T2 weighting) coronal and sagittal images. The menisci are the dark triangular structures in
A
marked with arrowheads. The normal posterior cruciate ligament is shown as a small black arrow in
A
and
B. C.
Proton-density coronal scan showing a large complex tear involving the posterior horn of the medial meniscus (black arrowhead) with most of the fragment displaced into the intercondylar notch (the “bucket-handle,” long black arrow) inferior to the normal posterior cruciate ligament.
D.
Sagittal proton-density image showing the meniscal fragment (long black arrow) displaced under the posterior cruciate ligament (short black arrow) and having a similar appearance (“double PCL sign”). Not shown is the “bucket” part of the meniscus, which stays attached to the medial tibia. (Reproduced, with permission, from Tintinalli, JE, Kelen GD, Stapczynski JS. Tintinalli’s Emergency Medicine: A Comprehensive Study Guide, 6th ed. New York: McGraw-Hill; 2004: Fig. 305-3A-D.)
9.
(E)
A flexion contracture as a sign of internal derangement of the knee at 10-14 days postinjury is an indication for an immediate surgical evaluation. Mechanical blocks of the joint are associated with higher complication rates such as permanent loss of normal range of motion and damage to articular cartilage from pinching and compression with knee joint movement. Therefore, although it would be helpful to expedite the MRI, if that seems unlikely to happen, it is appropriate to refer for an orthopedic consultation 10-21 days postinjury in the setting of a presumed mechanical block. The surgeon may recommend immediate arthroscopy to address the “locked” knee.