Headache Help (8 page)
Authors: Lawrence Robbins

HEADACHE HELP TIP: SWEETENING YOUR VISITS
If you’re going to a doctor for your headaches, chances are that you will have frequent visits, as you and your doctor explore what works and doesn’t work for you, to get prescriptions refilled, and get blood tests.
Personalize those visits
—
and get special attention from the staff
—
by bringing a treat, such as home-baked cookies, bagels and cream cheese, pastries from a local bakery, or a bag of candy. Not only does the treat lighten up the atmosphere at the doctor’s office, but you will make friends with the office staff and become a person instead of a name.
You might also do the same for your doctor: A Cornell University psychologist found that physicians make better decisions when they’re in a good mood, and that a little bag of candy or other token gift was all that it took to induce pleasant feelings. That positive effect can influence how your doctor solves problems creatively and makes decisions more efficiently.
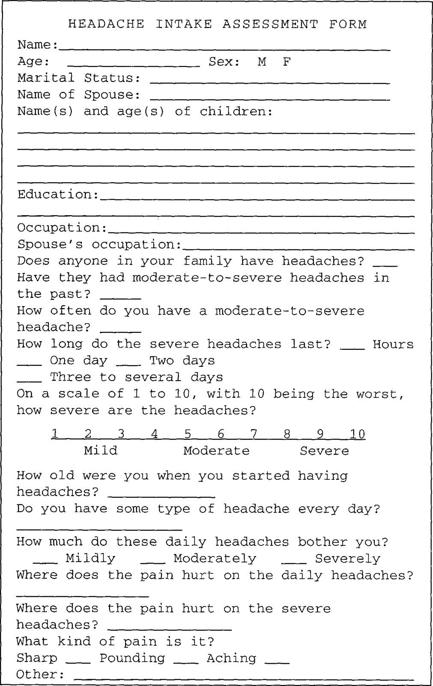
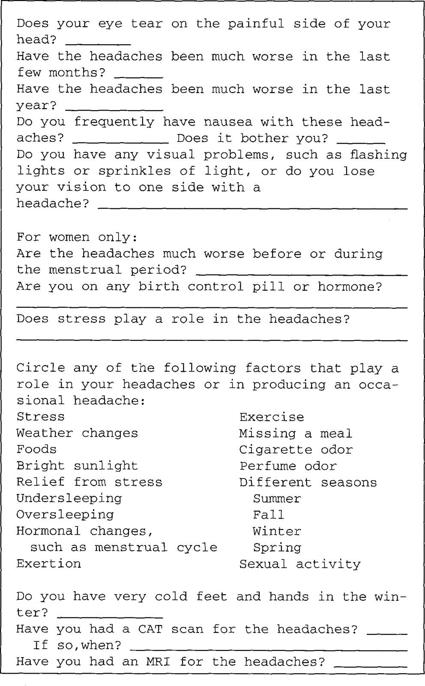
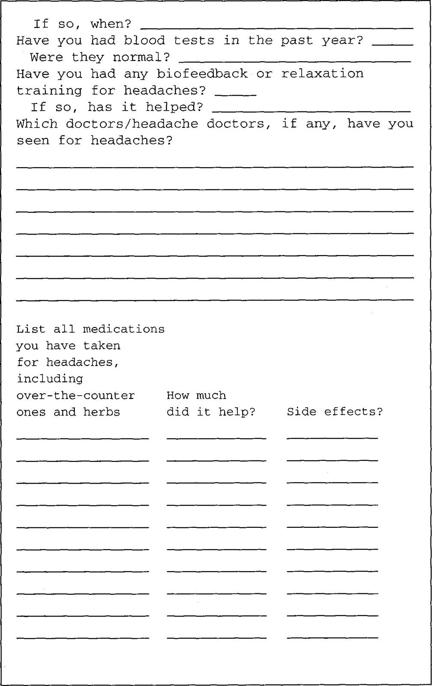
You need to tell the doctor about all medications and drugs that you are taking, including over-the-counter and illegal ones.
Keep track in list form of what you’ve tried and what happened and keep a list of other medications you take (and the dosages) for other conditions. Bring this information to each appointment. Be sure to keep the doctor informed about other medical problems you may have.
ON BEING A GOOD HEALTH CONSUMER
Although the doctor is responsible for making proper assessments and recommendations, it is more important than ever that consumers take an active role in their own healthcare. To help prevent mistakes, track your own medical care. The doctor may, for example, prescribe a medication that could have an ill effect on an ulcer condition. Perhaps you had a problem with an ulcer some ten years ago; that information may not be on the front page of the medical chart. It’s important for you to find out all you can about any new medication your doctor prescribes for you. Take responsibility by reviewing the drug information in this book or in reference books, such as the
Physicians’ Desk Reference.
Standard reference books on medications, available in most public libraries, list contraindications or conditions to watch out for with each medication. Be responsible for bringing a concern from your medical history to the doctor’s attention if it seems appropriate.
Also, the doctor may change the medication or dose for you over the telephone and neglect to make a notation of the change on your chart. Such mistakes happen. Doctors may also get sick or go on vacation, leaving a substitute who is unfamiliar with your case. If you can clearly convey the vital information the doctor needs, it will prove extremely helpful.
HEADACHE HELP TIP: SCHEDULING APPOINTMENTS
Consider scheduling your appointments for the first time slot in the morning or in the afternoon. By being first, you generally will not have to wait. If that’s not possible, call the office before you leave for your appointment to find out if the doctor is running late. That can save you a lot of frustration
—
and time!
ACCEPTING ONLY SATISFACTORY RELIEF
It is your responsibility to follow up with your physician if you experience ill effects from medications and need to deviate from what the doctor prescribed. Don’t give up if you come to a few dead ends. These are to be expected. Nevertheless, it’s reasonable to expect a medication to improve your headache situation from 50 to 90 percent.
4
Recognizing Migraines
T
HE TECHNIQUES
we’ve described thus far are most appropriate for preventing mild headaches or for keeping mild headaches from turning into severe ones. But for a chronic migraine sufferer, these techniques may fall short. A better understanding of migraines and migraine treatment will be essential for you to learn how to improve your quality of life.
Migraines can be devastating, with their sweeps of pain that can wipe out your ability to function and to think. Some 12 percent of us—about 18 percent of American women and 7 percent of men—are stricken at one time or another. Responsible for up to $15 billion in costs of absenteeism and billions more in diminished productivity and healthcare costs, migraines disrupt the lives of millions of Americans. Yet, to a great extent, these headaches remain underdiagnosed and undertreated.
In fact, according to a 1999 study sponsored by the National Headache Foundation, barely over half (53 percent) of people who suffer from migraines have ever been diagnosed by a doctor as having migraine headaches. Even more distressing is that only about one-third (34 percent) of migraine sufferers have ever consulted a doctor specifically about their severe headaches. Yet, three-quarters of migraine sufferers who have been treated appropriately report that the treatment has made a “dramatic improvement” in their quality of life.
WHO GETS MIGRAINES?
Most people who get migraines are probably born with a predisposition to them, which has been passed down from one generation to the next. At least four out of five migraine sufferers can identify a family connection, more than the sufferers of any other type of headache. Whether a person with an inherited predisposition actually gets frequent migraines depends on whether certain triggers (foods, bright lights, and so on, as explained in Chapter 6) aggravate his or her system enough to reach a threshold that sets off the migraine mechanisms.
Women are the most likely victims: they get migraines three times more often than men, probably because of all the hormonal changes they undergo.
Although migraines can strike at any age, most who are afflicted have well-defined migraines by their late teens and twenties, and then some get daily or almost daily tension headaches with occasional migraines later in middle age. These are called “transformed migraines” and add weight to the theory that migraines and tension headaches are part of the same headache spectrum. Some researchers believe that transformed migraines may actually be rebound headaches that develop from daily or almost daily use of over-the-counter medications, which turn sporadic headaches into frequent ones.
Occasionally, migraines and other kinds of headaches do begin in one’s fifties and sixties. If this is your experience, be sure to consult a physician because headaches can be a symptom of certain medical conditions that become more common with advancing age, such as certain brain disorders, arthritis, heart or kidney disease, high blood pressure, anemia, spine disorders, and respiratory illnesses. Although the chances are that the headaches do not stem from one of these problems, they should be excluded as possible causes.
One popular myth is that well-educated and wealthy people get more migraines. The truth is, these people just go to doctors more often. Lower-income women, in fact, have the highest risk of mi graines, perhaps because they endure more day-to-day stress trying to make ends meet. Stress, we’ll see time and again, is a powerful trigger in setting off migraines and other types of headaches.
YOU ARE NOT ALONE
If you get migraines, not only do you join more than 20 million live Americans, but some pretty famous dead people, too. Famous migraine sufferers have included Julius Caesar, Saint Paul, Thomas Jefferson, Frederic Chopin, Charles Darwin, Tolstoy, and Sigmund Freud. Supposedly, Lewis Carroll, who wrote
Alice in Wonderland,
might have been writing about what he felt or saw during a migraine aura.
Do people who get migraines have a certain stress-driven migraine personality? Some people think that a certain type of person—a perfectionist who is excessively critical of himself and others, and who gets angry but holds it in—is more prone to migraines. Yet most headache experts disagree. As we’ve said, migraines are inherited biochemical conditions or predispositions, much like asthma and heart disease, and not the result of a high-strung personality. The “gene” for migraines has been identified in several families.
WHAT ARE MIGRAINES?
Whether caused by a chromosomal defect or biochemical imbalances, migraines and their diagnoses are not clear-cut. Typically, you will get a diagnosis of migraines if you suffer from recurring moderate to severe headaches that are triggered by stress, certain foods, weather changes, smoke, hunger, fatigue, or other factors. More specifically, if you experience at least four of these features, the chances are that your headaches are migraines.
COMMON FEATURES OF MIGRAINES
- Recurrent: usually one to five times a month, but sometimes less. Last four to seventy-two hours, occasionally longer
- Triggered by a migraine-precipitating factor: stress, certain foods, weather changes, smoke, hunger, fatigue, and so on
- Sensitivity to light, regardless of head pain (Many sufferers wear sunglasses outside during all daylight hours.)
- Blurred vision
- Nausea or vomiting, which sometimes eases the head pain
- Sensitivity to noise
- Tenderness about the scalp, which may linger for hours or days after the headache pain is gone
- Early-morning onset (but may be anytime)
- Throbbing, pounding, aching, or pulsating pain, usually on one side of the face or skull and often behind an eye (though sometimes the pain moves)
- Cold hands and feet (not just when a migraine occurs) and occasionally a cold nose
- Prone to motion sickness (not just when a migraine occurs)
- Dizziness or lightheadedness
- Lethargy
- Fluid retention, with weight gain (Some people start retaining fluids before an attack and gain up to six pounds, but the weight gain is temporary.)
- Vertigo, occasional but potentially disabling, during an attack
- Anxiety
- A sensation of burning, prickling, tingling, numbness (paresthesia), often occurring in one hand or forearm, but may be felt in the face, around the jaw, or in both arms and legs
- Diarrhea, usually mild
- Visual disturbances or hallucinations (auras)
- Stuffy or runny nose
LESS COMMON FEATURES OF MIGRAINES
- Mild loss of ability to read, write, or even speak (aphasia)
- Confusion
- Fever, or moderate increase in body temperature
- Seizures (rare)
- Loss of muscular coordination (rare)
- Temporary paralysis (rare)