Digestive Wellness: Strengthen the Immune System and Prevent Disease Through Healthy Digestion, Fourth Edition (111 page)
Authors: Elizabeth Lipski

 Intestinal permeability testing
Intestinal permeability testing
 Lactose breath test
Lactose breath test
 Food sensitivity testing
Food sensitivity testing
 Avoid all gluten for at least three months.
Avoid all gluten for at least three months.
Avoid all gluten-containing grains and any products that contain them, even in small amounts. Gluten is found in many grains, including wheat (including couscous, semolina, orzo, bulgur, graham, and farina), rye, barley, millet, spelt, kamut, and triticale. Oats don’t contain gluten but are often contaminated with gluten from farming practices,
transportation, or manufacturing. In addition to obvious sources of gluten, many products have hidden sources. Salad dressings, some hot dogs, ice cream, bouillon cubes, chocolate, and foods containing hydrolyzed vegetable protein may contain gluten. (See
Chapters 9
and
10
for more information on gluten and gluten-free grains. Hidden sources of gluten can be found at
www.digestivewellness.us
.)
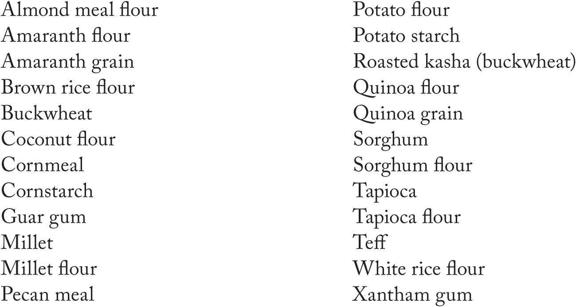
Gluten-free grains and grain substitutes include:
Although giving up gluten will be difficult at first, it has become easier over the past few years with the growing number of products, restaurants, and bakeries offering gluten-free options. You’ll be able to find delicious breads, pastas, cookies, crackers, and more.
 Try digestive enzymes.
Try digestive enzymes.
Either pancreatic or vegetable enzymes can be used to enhance digestive function. Take one to two with each meal. Specific amylase enzymes can be of particular benefit.
 Supplement with probiotics.
Supplement with probiotics.
Probiotic flora enhances digestive function. Either eat cultured and fermented foods or take probiotic supplements.
 Try gut-healing nutrients.
Try gut-healing nutrients.
Glutamine, N-acetyl-D-glucosamine, and gamma oryzanol, are all healing to the intestinal lining. While no specific testing has been done on therapeutic use of these nutrients in people with celiac disease, clinical experience with celiac indicates their usefulness.
 Take a multivitamin with minerals.
Take a multivitamin with minerals.
Zinc, selenium, folic acid, iron, and vitamins A, B
6
, D, E, and K have all been shown to be deficient in people with celiac disease. Get a good-quality multivitamin with minerals. Look for a supplement that is hypoallergenic and contains no grains or dairy.
25
The Colon or Large Intestine
Common problems in the large intestine, also called the colon, include constipation, diarrhea, diverticular disease, irritable bowel syndrome, inflammatory bowel disease, ulcerative colitis, Crohn’s disease, hemorrhoids, polyps, and colon cancer. Proper functioning of the colon requires a high-fiber diet. The colon is home to tens of trillions of beneficial bifidobacteria and other flora that ferment dietary fiber that, in turn, produce short-chain fatty acids, butyric acid, valerate acid, propionic acid, and acetic acid. These short-chain fatty acids are the primary fuel of the colonic cells. They’re needed to maintain, fuel, and build new colonic cells. Without adequate fiber, we starve the colonic cells and weaken the integrity of the colon. Butyric acid has been shown to stop the growth of colon cancer cells in vitro and is used clinically to heal inflamed bowel tissue.
The colon’s main function is to recycle nutrients and water back into our bodies and eliminate waste products. Adequate hydration is essential for good colon health. Water is our best choice, followed by fresh vegetable juices, diluted fruit juices, herbal teas, coconut water, and fruits and vegetables.
Constipation affects up to 28 percent of North Americans. Physicians write more than a million prescriptions for constipation relief annually, and we spend $725 million a year on laxatives. Constipation is defined differently by different people, and
it is often subjective: I feel constipated if I have only one bowel movement a day. The Rome III criteria for constipation includes two or more of the following: straining at least 25 percent of bowel movements; lumpy or hard stools at least 25 percent of the time; sensation of incomplete evacuation in at least 25 percent of bowel movements; sensation of obstruction at least 25 percent of the time; manual maneuvers to facilitate evacuation at least 25 percent of the time; fewer than three bowel movements a week. An additional symptom is hard stools unless you use laxatives. The Rome III criteria attempt to differentiate between constipation and constipation-type IBS, but the latest research indicates that these are artificial divisions that aren’t really useful. Constipation affects women twice as often as men and is more common in people over age 65.
Fifty percent of people have bowel movements daily; many people do not have a bowel movement every day; most people are irregular and may not have the same number of bowel movements every day or at the same time of day. In integrative circles, it is considered normal to have one to three soft bowel movements each day. Optimal bowel transit time is 12 to 24 hours, so if you are having only three bowel movements each week, you have a transit time of 56 hours, which is way too long. This makes sense in light of current theories about fecal transit time. If you haven’t done the transit time self-test, now would be a good time. (See section on bowel transit time in
Chapter 2
.)