Brain Lock: Free Yourself From Obsessive-Compulsive Behavior (12 page)
Read Brain Lock: Free Yourself From Obsessive-Compulsive Behavior Online
Authors: Jeffrey M. Schwartz,Beverly Beyette

In Tourette’s syndrome, a disease that is genetically related to OCD, the person develops chronic multiple tics, or sudden movements and vocalizations that occur almost without warning. The problem—as we believe it to be with OCD—is that the striatum is not properly modulating the cortex. Furthermore, scientists know that people who have damage to their basal ganglia or to the front part of their brain will perform a behavior over and over, even when that behavior is no longer useful or, indeed, is detrimental to them. The person with OCD performs a ritual in response to an obsession, all the while knowing it makes no sense. As with these other conditions, we believe this is due to a malfunction in the modulation of the cortex by the automatic transmission and filtering systems of the basal ganglia or striatum.
Whereas one person in forty in the general population has OCD, OCD occurs in one out of five family members and relatives of those with Tourette’s syndrome and in one-half to three-fourths of those with Tourette’s syndrome themselves, lending credence to the theory of genetic association. Frequently, Tourette’s victims develop painful arthritis or tendonitis in their joints because of the intense jerking movements that motor tics cause. In essence, they get a strong intrusive urge to move and then perform tics to relieve themselves of the discomfort. Or they may get vocal tics, starting with an urge to do repetitive throat clearing, an urge that may later develop into yips, yelps, barks, or other animal sounds. Or they may start screaming obscenities or racial slurs involuntarily, causing them great stress. Stress makes the urges much worse, as it does in OCD. Preliminary data from our PET scans at UCLA indicate that the putamen, the part of the striatum that sits next to the caudate nucleus and modulates body movements, alters metabolic function in persons with Tourette’s syndrome. Many people with OCD also have motor tics, and a lot of people with Tourette’s syndrome get compulsive symptoms. What is common to both, we now believe, is that parts of the cortex—probably the motor cortex in tics and the orbital cortex in obsessions and compulsions—are not being properly modulated by the appropriate parts of the striatum (problems in
the putamen are related to tics, and problems in the caudate nucleus are related to OCD symptoms). Thus, problems in two closely related brain structures that modulate and filter movement or thought seem to underlie two genetically related conditions that cause difficulty with intrusive movements (tics) in Tourette’s syndrome or thoughts (obsessions) in OCD.
THOSE PRAGMATIC PRIMATES
The front part of the brain is where sophisticated information processing and problem solving take place. Because of the nature of the brain structures that send signals to the underside of the front of the brain—the orbital cortex—it seems likely that problem solving that involves emotional issues may take place there. A study by E. T. Rolls, a behavioral physiologist at Oxford University in England, yielded some interesting data that may be relevant for understanding the brain’s role in symptoms common to persons with OCD.
Rolls wanted to find out what is really going on in the brain when repeated inappropriate behaviors, or behavioral perseverations, are occurring, so he had rhesus monkeys trained to do a simple visual task. For example, the monkeys learned that every time they saw a blue signal on a screen, they would be rewarded with black currant juice if they licked a little tube. Now, monkeys really like juice and will work hard to learn behaviors that promise this reward. So the monkeys learned fast: When the blue color appeared—bingo!—juice was in the tube. Thus, the monkeys worked along happily and efficiently, licking the tube at the proper time. Through electrodes that had been placed in the monkeys’ brains, Rolls was able to observe that once the monkeys understood that a certain color signaled that juice was coming, cells in their orbital cortex would fire as soon as that color appeared. So the orbital cortex clearly was able to “key in” on signals that meant “juice is coming.”
Rolls knew that just as monkeys love juice, they hate the taste of salt water. When he offered the monkeys a syringe filled with salt water, they made the connection—syringe/salt water—and soon the mere sight of the syringe caused other nearby cells in the orbital cortex to fire to help the monkeys back off and avoid the salt water. So,
there are cells in the orbital cortex that fire when there’s something you want—and when there’s something you want to avoid. It’s pretty clear that the orbital cortex was involved in the monkeys’ learning quickly to recognize environmental stimuli and to signal the monkeys, “Hey, this is something you want. This is something you don’t want.”
Next, Rolls wanted to see what would happen when he tripped up the monkeys. Now the monkeys had to learn that it was the green signal, not the blue signal, that would get them the juice. On the first trial, when the monkeys licked the little tube for the blue signal and came up with salt water instead of juice, other cells in their orbital cortex fired much more intensely and with much longer bursts than the cells that had fired when things were going as they had come to expect.
It’s important to note that these cells in the monkeys’ brains that fired in long bursts did not respond to the taste of salt water outside the test situation. What they were responding to was the fact that the monkeys had made an error. In fact, the orbital cortex fired even when the monkeys received nothing at all at times when they expected juice. After another trial or two, the monkeys stopped licking the tube for the blue signal. They learned quickly that this signal was no longer getting the job done and that it was the green signal they wanted. And, as the monkeys consistently licked the little tube for the green signal, those orbital cortex cells that fired for the winning color started firing for the green signal instead of the blue signal. So what was happening, it seems, was that as the monkeys learned that they had been double-crossed and now had to change their behavior to get the juice they craved, the orbital cortex made a change to help them quickly recognize that green was now the winning signal. The orbital cortex is able to recognize both right answers and wrong answers. It is a genuine “error-detection system”—and it’s the wrong answers that make it fire in long, intense bursts.
Rolls speculated recently that these “error-detection” responses in the orbital cortex could be involved in emotional responses to situations that cause frustration. It seems reasonable that activity in the orbital cortex may be related to an internal sense that “something is wrong” and needs to be corrected by a certain behavior. The monkeys responded by changing their behavior. In OCD patients, this
error-detection circuit may become chronically inappropriately activated—or inadequately inactivated—perhaps because of a malfunction in the filtering effects of the basal ganglia. The result could be persistent intrusive thoughts and sensations that something is amiss. The cingulate gyrus, interacting closely with both the orbital cortex and the caudate nucleus, could greatly amplify this internal, gut-level feeling of dread.
The monkey experiment helped us understand why people whose orbital cortex is damaged have problems with perseveration. If the error-detection system is broken, people have trouble recognizing mistakes and tend to repeat the same old habits over and over again. But Rolls’s experiment with the monkeys also helped us understand what’s going on with OCD. Remember, when the monkeys saw something they didn’t want, the orbital cortex fired, sending out a signal: “That’s no good—something’s wrong.” But what made the orbital frontal cortex fire
really
intensely was when the monkeys made an error because the blue signal was no longer associated with the juice. The orbital cortex firing intensely can give a strong feeling that “something is wrong.” If the error-detection system keeps firing over and over, it can cause a chronic intense feeling that “something is wrong” and lead a person to do desperately repetitive behaviors to try to make the feeling “get right.” What may cause this? We know that the error-detection system in the orbital cortex is strongly connected to the caudate nucleus, which modulates it and can turn it off by causing a shift of gears to another behavior. There is now excellent evidence from a variety of scientific studies that damage to the basal ganglia (of which the caudate nucleus is a part) can cause OCD, with its terrible feelings that “something is wrong,” feelings that don’t go away.
The end result of a caudate nucleus problem can be that the error-detection system gets stuck in the ON position, leading to a something-is-wrong feeling that will not go away. Our theory is that since the orbital cortex is modulated by the caudate nucleus, when the caudate nucleus modulation isn’t working right, the error-detection system in the orbital cortex becomes overactive, and the person has terrible thoughts and feelings that “something is wrong,” which lead to compulsive behaviors done in a desperate attempt to make the feelings go away. Unfortunately, these repetitive behaviors make
the something-is-wrong feelings even more intense. The only way to break the vicious cycle is to change the behavior. As you’ll see, this may also be where medication can be helpful.
The important role of the orbital cortex in OCD’s terrible urges and compulsions is being documented more and more. In a recent study at Massachusetts General Hospital, PET scanning was used to measure blood-flow changes in persons with OCD. Researchers put each person in a scanner with a dirty glove or some other object that was sure to be very upsetting, and the person had to lie there with the dirty glove, fretting and worrying about contamination. What these researchers saw was a clear increase in orbital cortex activity, especially on the left side, when the patient’s OCD got worse.
This finding is of particular interest because we now have data indicating a relationship between a change in left orbital cortex metabolism and treatment response in OCD patients. In our experiment at UCLA, drug-free patients were given PET scans, undertook ten weeks of cognitive-behavioral therapy, and were then scanned again. Post-therapy, there was a highly significant correlation between decreased metabolic activity in the left orbital cortex and a lessening of OCD symptoms. The patients who showed the most improvement had the most clear-cut decrease in left orbital cortex metabolism. It was behavior therapy alone, without drugs—the same method I’m teaching you in this book—that caused the change.
UNLOCKING YOUR BRAIN
What we have also learned at UCLA is that people with OCD have what amounts to “Brain Lock” on the right side of the brain. When a person with OCD is symptomatic, the metabolic activity rate not only increases in the orbital cortex, but locks together with the activity in the caudate nucleus, the thalamus, and the cingulate gyrus. The activity in all these parts is locked together, so that changes in the orbital cortex are tightly linked to changes in activity in the other three. Behavior therapy is the key that unlocks them and allows them to work freely again. Do your therapy, unlock your brain. Add the “waterwings” (the medication), and the response rate soars to 80 percent.
We have shown that we can literally make a new brain groove. As
people with OCD apply themselves to behavior therapy, abandoning the inappropriate perseverational behaviors and responding to OCD urges and thoughts with positive, nonpathological behaviors, we see changes in the orbital cortex and in the striatum. We see Brain Lock alleviated; the circuitry has shifted. The next step is to get that new circuitry to become more functional, more automatic. As the circuitry becomes automatic, the striatum shifts gears and runs the circuitry properly because that is what the striatum normally does.
Change the behavior; create a new groove; get behavioral improvement; and, in time, you will change your brain and get relief from OCD symptoms
.
We studied eighteen subjects and found that within ten weeks, twelve demonstrated significant clinical improvement. All were treated as outpatients. None took medication. There were three main findings.
- Those who did respond showed significant decreases in caudate nucleus metabolism that were present on both sides of the brain, but were more robust on the right side (as in Figure 3, opposite).
- Whereas before treatment there were significant correlations of brain activity among the orbital cortex, the caudate nucleus, the cingulate gyrus, and the thalamus on the right side—Brain Lock—these correlations decreased significantly, which means that the Brain Lock was alleviated.
- There was a strong correlation between the amount of metabolic change on the left side of the orbital cortex and percentage changes in patients’ scores on severity ratings of OCD symptoms. That is, the more the OCD improved, the more the orbital cortex tended to “cool down.”
These findings demonstrate conclusively that it is possible to make systematic changes in brain function with self-directed cognitive behavior therapy alone.
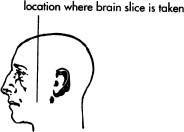
Figure 3. PET scan showing decreased energy use in the right caudate nucleus (which appears on the left side in a PET scan) in a person with OCD after successful treatment with the Four-Step Method. PRE shows the brain before and POST ten weeks after behavioral therapy with no medication. Note the decrease in “size,” which signifies decrease in energy use, in the right caudate (rCd) after doing the Four-Step Method. The drawings show where the caudate nucleus is located inside the head.