Pediatric Examination and Board Review (104 page)
Read Pediatric Examination and Board Review Online
Authors: Robert Daum,Jason Canel

FIGURE 63-3.
Strabismus (squint). This term refers to disorders in which the optic axes are not parallel. The diagrams illustrate positions of the patient’s eyes as they appear to the observer. The unbroken circles connected by the unbroken lines show pairs in the primary position with the normal or fixing eye represented in heavier lines. Pairs with broken lines are in secondary positions with the heavier lines for the fixing eye.
A.
Comitant strabismus: the squint angle between the two optic axes is constant in all positions regardless of which eye fixates.
B.
Right lateral rectus paralysis: the right eye is unable to move laterally.
C.
Right medial rectus paralysis: the right eye is lateral in the primary position; it fails to move medially.
D.
Right superior rectus paralysis: the right eye is slightly depressed in the primary position and fails to move farther upward.
E.
Right inferior rectus paralysis: the right eye is elevated slightly in the primary position; it cannot move downward. (Reproduced, with permission, from LeBlond RF, DeGowin RL, Brown DD. DeGowin’s Diagnostic Examination, 9th ed. New York: McGraw-Hill; 2009: Fig. 7-35.)
7.
(A)
8.
(C)
He most likely has an accommodative esotropia, which most commonly presents between 2 and 3 years old as a new-onset esotropia. Family histories of amblyopia are common. The great majority of these children have an associated hyperopia, and their esotropia is because of overaccommodation in response to the hyperopia. Treatment of the hyperopia is indicated first (with prescription eyeglasses) (see
Figure 63-4
).
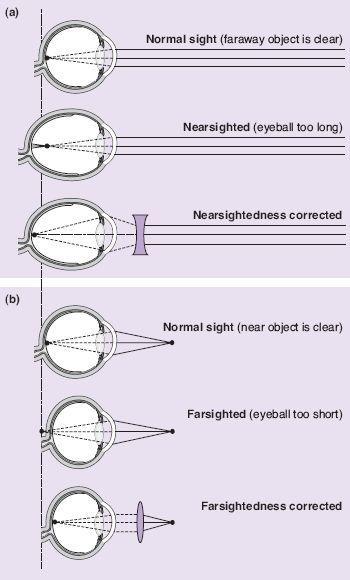
FIGURE 63-4.
Common defects of the optical system of the eye. In hyperopia (farsightedness) the eyeball is too short and light rays come to a focus behind the retina. A biconvex lens corrects this by adding to the refractive power of the lens of the eye. In myopia (near-sightedness) the eyeball is too long and light rays focus in front of the retina. Placing a biconcave lens in front of the eye causes light rays to diverge slightly before striking the eye so that they are brought to a focus on the retina. (Reproduced, with permission, from Widmaier EP, Raff H, Strang KT: Vander’s Human Physiology, 11th ed. McGraw-Hill, 2008:211.)
9.
(D)
Strabismus can be found in healthy infants until age 3-6 months, at which time the inability to follow a target symmetrically resolves. Ophthalmology referrals are needed for children with genetic syndromes, in utero drug or alcohol exposure, infants with retinopathy of prematurity (a 26-week gestation premature infant would most likely have this), children who have evidence of ocular pathology on examination, and children with a strong family histories of vision difficulties.
10.
(E)
When measured by visual evoked potential, newborns have visual acuity of approximately 20/400.
11.
(D)
Peg-in-hole games are visually related behaviors that should suggest to the practitioner possible vision impairment if this milestone is not achieved on time. By 8-9 months, a child should poke at the holes with pegs and by 12-14 months should be able to put pegs into the appropriate holes. Infants should smile at 2-3 months, and fix and follow by 2-3 months (by 2 months it is a red flag; by 3 months an absolute referral). Strabismus is referred to ophthalmology after 6 months. All children are mildly hyperopic until approximately 10 years old.
12.
(C)
13.
(A)
14.
(B)
15.
(D)
The most advanced test of visual acuity possible should be used for a child’s developmental age. The Allen cards are a series of familiar object cards that the child is asked to identify at increasing distances. The appropriate vision screening tools for ages 3-5 years are the matching-type tests, namely the HOTV test (chart on wall with letters H, O, T, V and child holds matching cards) and the tumbling Es (chart on wall with the letter E in various rotations and child holds matching cards).
16.
(D)
This patient by history has myopia, nearsightedness, which is causing her to strain to see far objects—squinting in the car or pulling objects closer to her face to see them more clearly. The presence of clinical symptoms for some time suggests the need for a higher diopter on examination (see
Figure 63-5
).
17.
(A)
Almost all infants are born with slight hyperopia that increases throughout childhood, peaks at approximately 6 years old, and then decreases again. Most myopia is physiologic as opposed to pathologic.
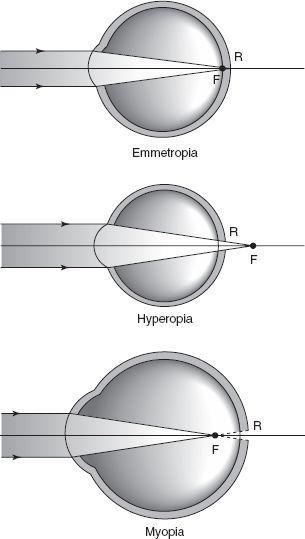
FIGURE 63-5.
Spherical refractive errors as determined by the position of the secondary focal point with respect to the retina. (Reproduced, with permission, from Riordan-Eva P, Whitcher JP. Vaughn & Asbury’s General Ophthalmology, 17th ed. McGraw-Hill; 2008: Fig. 20-21.)
18.
(D)
The AAP and the American Academy of Ophthalmology recommend routine visual acuity testing at 3 years and again at 5-6 years. Screening for eye disease should be performed regularly, at least in the first 3 months of age and again at 12 months.
 S
S
UGGESTED
R
EADING
Behrman RE, Kliegman RM, Jenson HB, et al.
Nelson Textbook of Pediatrics
. Philadelphia, PA: WB Saunders; 2007.
Committee on Practice and Ambulatory Medicine; American Academy of Ophthalmology. Eye examination in infants, children, and young adults by pediatricians.
Pediatrics.
2003;111(4):902-907.
Curnyn KM. The eye examination in the pediatrician’s office.
Pediatr Clin North Am.
2003;50(1):25-40.
Guthrie ME. Congenital esotropia.
Ophthalmol Clin North Am.
2001;14(3):419-424.
CASE 64: A 4-YEAR-OLD WITH A NECK MASS
A 4-year-old comes to your office with his father because of a “lump in the neck” that his parents noted 4 days earlier. The boy does not seem bothered by it, and although he is not currently ill, he did have a “cold” about 1 week ago. He has not had a fever, is eating and drinking well, has no specific tooth pain, and no pain on swallowing.
On examination he is afebrile. His oropharynx is normal, nares clear, and his conjunctivae are white. He has a tender 4-cm submandibular lymph node on the left side that has overlying erythema. His abdominal and skin examinations are normal.
SELECT THE ONE BEST ANSWER
1.
What is his most likely diagnosis?
(A) cat-scratch disease
(B) “atypical” or environmental
Mycobacterium
infection
(C) acute lymphadenitis
(D) mumps
(E) tuberculosis (TB)
2.
What is the
least
likely pathogen causing his illness?
(A) “atypical” or environmental mycobacteria
(B)
Streptococcus pyogenes
(group A streptococci)
(C)
S aureus
(D) EBV
(E) anaerobic bacteria
3.
What antibiotic will you prescribe for him?
(A) IM ceftriaxone
(B) oral (PO) azithromycin
(C) PO amoxicillin
(D) PO cephalexin
(E) PO amoxicillin-clavulanate
4.
Which of the following are also known to cause cervical lymphadenopathy?
(A) Non-Hodgkin lymphoma
(B) Kawasaki disease
(C) systemic lupus erythematosus
(D) A and B
(E) A, B, and C
5.
You are called by the parents of a 2-week-old newborn boy, who report poor feeding for 1 day and some neck swelling on the right side. On examination you note a well-hydrated, fussy but consolable infant with a temperature of 101.2°F (38.4°C) rectally and a right-sided 2 × 4-cm spongy, tender neck mass with overlying erythema. The rest of the examination is normal. What are the possible etiologies of the neck mass in this child?