Read Outbreak! Plagues That Changed History Online
Authors: Bryn Barnard
Outbreak! Plagues That Changed History (6 page)

In 1804, Haiti declared itself a republic. In 1816, the new nation helped the South American general Simón Bolívar mount the invasion that ultimately ended the Spanish empire in the Americas. In return, Bolívar promised to free his own slaves and outlaw slavery in the lands he liberated.
Elsewhere in the Caribbean and the southern United States, slave revolts increased. So did repressive legislation designed to keep slaves in their place, and an abolitionist movement to set them free. One ahead-of-his-time British planter suggested that rethinking the slavery “brand” would solve the problem. Call them “plantation assistants,” he suggested, and abolitionists would stop complaining. No one yet realized that with a free Haiti as an example, slavery was finished in the Western Hemisphere. Abolitionist pressure killed British slavery in 1838. The American Civil War drove a stake through the heart of American slavery in 1865. No one thanked yellow fever for starting the revolution.
Even after the demise of slavery, yellow fever continued to have an impact on the New World. In 1881, French engineers began construction of a sea-level canal through the Isthmus of Panama. The project was led by renowned French diplomat-impresario Count Ferdinand de Lesseps, who had successfully managed the construction of the Suez Canal across Egypt. Unlike Egypt, however, Panama had a deadly reputation for both malaria and yellow fever. De Lesseps downplayed this problem. To reduce miasmas still thought to cause the disease, the French built tidy, clean, well-built worker barracks with elaborate ornamental gardens. Even before construction began, however, workers started dying from malaria and yellow fever. Since miasma was accounted for, a variety of sin-based explanations were proposed: drinking, gambling, even embezzling were all suspected of causing disease. One engineer, out to prove that immorality was the culprit, brought his upstanding family to Panama. Yellow fever killed them all. Finally, in 1889, with thirty thousand workers dead, billions spent, the canal unbuilt, and de Lessep’s reputation in tatters, the project was abandoned.
In 1880, a year before de Lesseps embarked on his Panamanian folly, Dr. Carlos Finlay suggested that
Aedes
mosquitoes might transmit yellow fever. Finlay observed that healthy humans bitten by mosquitoes that had previously fed on yellow fever sufferers also caught the disease. Finlay’s hypothesis was ignored for decades, but he was exactly right.
In essence, a mosquito is an airborne syringe. Mosquitoes are equipped with a long hollow proboscis for drinking liquids, a tube for injecting saliva, and a set of cutting stylets for making a wound. Only females use this apparatus to drink blood, and then only when they need to nourish egg production. (For regular meals, mosquitoes drink nectar or honeydew.) When females need a blood meal, they land on a host, poke a hole through the skin, nick a capillary, inject some anticoagulant to make the blood flow, and drink up. Of the 2,500 kinds of mosquitoes, most prefer to dine on other animals. Only a small minority vampirize people. Of the deadly illnesses mosquitoes carry, only a handful affect us. But they’re doozies, including ma-laria, dengue fever, encephalitis, West Nile virus, and yellow fever. Since the Stone Age, the mosquito has probably killed more people than any other creature.
In 1900, during the Spanish-American War, the mystery of yellow fever was finally unraveled. Thousands of American soldiers engaged in the conquest of Cuba had already died from yellow fever when a medical team led by Major Walter Reed arrived to try to determine the cause of the disease. Reed joined three other physicians already at work in Cuba: Jesse Lazear, Aristides Agramonte, and James Carroll. Lazear believed in Carlos Finlay’s mosquito-transmission idea. Reed was dubious but allowed Lazear to test the hypothesis. Carroll volunteered to be bitten by a mosquito that had fed on a yellow fever patient. He got sick and recovered. Needing further proof, Lazear allowed himself to be bitten. Two weeks later, he was dead. On October 23, 1900, Walter Reed announced that the
Aedes aegypti
mosquito was
the insect vector (transmitter) for yellow fever.
In Cuba, once the mosquito vector was confirmed, Major General William Crawford Gorgas was charged with its destruction on the island. The female
Aedes
mosquito prefers the moist edges of artificial water containers to lay her eggs. The casks of drinking water taken on board slave ships departing from Africa had transported
Aedes
to the Americas. Now ponds, flower vases, old tires, and other water containers were sustaining the disease. Soldiers under Gorgas’s super-vision emptied or smashed water containers and sprayed oil on ponds where
Aedes
might breed. Within five months, these methods had eliminated yellow fever from Cuba. Gorgas was a hero. In 1904, he was dispatched to the American revival of the Panama Canal project. By 1906, using the same methods, Gorgas had eradicated yellow fever there, too.
It would not be until 1927 that the South African physician Max Theiler and his colleagues would prove that yellow fever was caused by a Flaviviridae virus and eventually develop a successful vaccine. Called 17D, it is still used today. Later, scientists learned where yellow fever hid in between epidemics: the African virus has found a permanent reservoir in the New World tropics among populations of tree-dwelling monkeys and their mosquito parasites. High above humans in the forest canopy, the virus cycles between insect and animal. As long as the forest is undisturbed, yellow fever remains “silent” for years or even decades. But each time a tree is cut to clear more land for habitation or agriculture, yellow fever may crash back to earth, ready to reenter the human population chain.
The Flaviviridae virus
But what about yellow fever’s impact in the white man’s grave? Africans suffered from the disease but were not insensitive to its deadly effects on their colonial masters. While whites saw yellow fever as an obstacle to control, Africans recognized it as an ally in their struggles for freedom and independence. Well into the 1980s, these words were still chanted by many African schoolchildren: “… Only mosquito can save Africa. Only malaria can save Africa. Only yellow fever can save Africa.”
The African Flaviviridae virus has found a permanent reservoir in tree-dwelling New World primates, like these howler monkeys, and their mosquito parasites. When the tropical rain forest is cut down, the pathogens of the canopy may come into contact with people, giving yellow fever a chance to reenter the human infection chain.
You know the drill: wipe, wash, don’t forget to flush. We learn the habits of personal hygiene from our parents, in school, on the job, and from the media. They seem basic, natural, obvious—even scientific. But they didn’t start that way. A little over a century ago, cleanliness and sanitation were still radical notions resisted by just about everyone. It took several global pandemics to change people’s habits.
In 1817, a new disease swept out of India. It caused a violent, gushing diarrhea and vomiting that within a few hours could turn a healthy human being into a shriveled, blue-tinged corpse. No one knew what caused the illness. No one understood how it was spread. What people
did
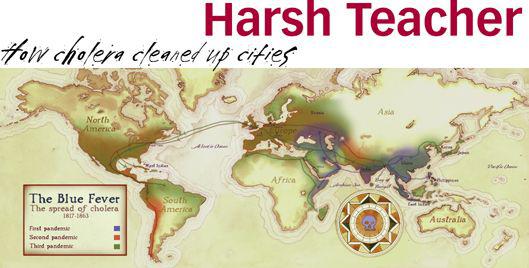
know was that it didn’t discriminate: rich or poor, anyone who contracted the disease was likely to die. In seven separate pandemics over 180 years, it traveled to every continent except Antarctica, killing millions of people. Along the way it was given many names: hyperanthraxis, spasmodic cholera, Asiatic cholera, convulsive nervous cholera, cholera asphyxia, malignant cholera, the blue cholera, the blue fever, the blue vomit, the yellow wind, the plague, the pestilence, the black illness.
Today we call it simply cholera. Simply put, it has been one of the most influential diseases of modern times. Cholera highlighted the desperate poverty and ghastly living conditions of newly industrialized Europe and America. It laid bare the threads connecting poverty to wealth. It settled the argument between two contending theories of disease, miasma and contagion. Most importantly, it catalyzed the development of modern sanitation, which enabled huge numbers of people to live together in close quarters and remain healthy, making the modern city possible. Sanitation is also partially responsible for the human population explosion. About one billion people inhabited our planet in 1800. We’re over six billion and counting today.
For most of the nineteenth century, people didn’t know what caused cholera.
Miasmists
—followers of the ancient theories of Galen—blamed the disease on mysterious emanations: electrical currents (“the miasmic electric effluvium”), rotting garbage, foul-smelling sewers, and puzzling swamp vapors.
Contagionists
believed cholera was spread by contact with an infectious agent: bad cucumbers, bad beer, foreign food, shellfish, phosphorus, copper, sulfur, or other contaminants.
Nineteenth-century industrial cities were fetid sties, mounded with garbage and human waste. Rivers served as both sewers and sources of drinking water, spreading cholera and other diseases. People died at rates rivaling those associated with the Black Death.
Cures and preventatives were varied and contradictory. Several towns tried quarantines. Others experimented with noise: cannons were blasted, muskets fired, gongs banged, and shouts raised from sunrise to sunset. Several nations tried closing their borders to all travelers. Many individuals tried waist-hugging flannel cholera belts. Entrepreneurs made fortunes selling cholera brandy and cholera drops. Doctors prescribed hot poultices of salt, mustard,
roasted black pepper, powdered ginger, scraped horseradish, or burnt cork. They also recommended ice-water baths, boiling-water baths, tobacco enemas, opium suppositories, and the ever-popular phlebotomy. England twice tried a National Day of Prayer and Deliverance. Nothing worked.



